Act Now

Empower U: Learn to Access Your Disability Rights Training on Canadian Human Rights, the Convention on the Rights of Persons with Disabilities (CRPD) and its Optional Protocol (OP) training aims to increase awareness of how to address discrimination using more familiar Canadian human rights laws such as Human Rights Codes and the newer international Convention on the Rights of Persons with Disabilities (CRPD). This is training for persons with disabilities by persons with disabilities. The training is part of a project funded by Employment and Social Development Canada and implemented by the Council of Canadians with Disabilities (CCD) in collaboration with Canadian Multicultural Disability Centre Inc. (CMDCI), Citizens With Disabilities – Ontario (CWDO), Manitoba League of Persons with Disabilities (MLPD) and National Educational Association of Disabled Students (NEADS). Read more.
Sign Up for our monthly digest
A monthly newsletter from CCD about what is happening in the community
Legalizing Physician-Assisted Death: Can Safeguards Protect the Interests of Vulnerable Persons?
Related Documents
February 26, 2024
C-62: CCD, ARCH, Inclusion Canada, DAWN Canada Urged Changes to MAiD Bill - February 23, 2024
November 25, 2021
An Open Letter from the Council of Canadians with Disabilities (CCD) Concerning the Canadian Psychiatric Association Position Statement on Medical Aid in Dying (MAiD)
March 15, 2021
CCD Disappointed by House of Commons Yes Vote on Bill C-7 (Medical Aid in Dying)
PREPARED FOR THE COUNCIL OF CANADIANS WITH DISABILITIES BY ORVILLE R. ENDICOTT UNDER THE SPONSORSHIP OF THE CANADIAN BAR ASSOCIATION "LAW FOR THE FUTURE FUND"
2003
FOREWORD
This study of the issues involved in the legalization of physician-assisted death has been undertaken at the request of the Council of Canadians with Disabilities. It has been supported financially by the Canadian Bar Association "Law for the Future Fund". The views expressed here are not necessarily those of either the Council of Canadians with Disabilities or the Canadian Bar Association.
Table of Contents
II. Indicators of the devaluation of the lives and freedoms of persons with disabilities
III. What needs to be guarded against?
V. Safeguards in Current Canadian Law
VI. Processes and Proposals to Review and Change Canadian Law
A. Senate Committee on Euthanasia and Assisted Suicide
B. Senate Subcommittee Update of Life and Death - June, 2000
C. Other legislative proposals
VII. Developments Outside Canada
A. United States litigation
B. Oregon's Death with Dignity Act
C. United States Federal Pain Relief Promotion Bill
D. Netherlands practices and legislation
E. Northern Territory of Australia's Rights of the Terminally Ill Act
F. Proposed legislation in other countries
VIII. Analysis and Conclusions
A. Issues, realities, principles and cautions
B. In what kind of a society might it be safe to legalize assisted death?
C. Prosecution of health care providers
D. Procedural safeguards
E. Criteria: who is qualified to receive assistance in dying?
F. Conclusion
EXECUTIVE SUMMARY
- This study explores the two interrelated problems confronting persons with disabilities in a society that tolerates assisting people to die before a terminal illness takes its course: the unwanted and/or unwarranted loss of one's life, and the loss of personal autonomy in making end-of-life decisions. It examines various types of safeguards that might be employed to reduce or eliminate these risks.
- "Assisted death" is understood to include assistance to end one's own life ("assisted suicide"), and both active and passive euthanasia, involving a decision made by the individual or a surrogate decision maker, but also involving the co-operative action of an outside agent, ordinarily a health care practitioner. "Active" euthanasia consists of the administration of a lethal substance or other act intended to bring about the death of a person. "Passive" euthanasia consists of the withdrawal or withholding of a potentially life-sustaining procedure, again with the intention of hastening the individual's death.
- Having a disability often leads to the devaluation of the life of an individual, and consequently makes other people think that he or she would be better off dead. Although the individual might value his or her own life as much as anyone else would, knowing that others assign diminished value to one's life can affect the voluntariness of any decision to seek assistance in dying. Substitute decision makers are likewise influenced by the pervading view that the life of a person with a disability is a life not worth living.
- Safeguards against such abuses can take several forms. For example, some are direct, such as prohibition of certain acts; others are indirect, such as the development of better therapeutic and pain relieving procedures and medications and the provision of social supports, which would make recourse to assisted death a less desirable option. Some safeguards could precede a person's death and thus prevent a wrongful choice, while others may follow after one person's death (criminal prosecution or disciplinary proceedings, for example) and make such a choice less likely for other persons.
- There is a considerable body of public opinion in Canada and elsewhere that ending the life of a person with a disability is much less blameworthy than killing a person who does not have a disability. Often the killing of a person with a disability is characterized as "mercy killing", regardless of whether the individual was experiencing severe pain. There have been calls for a new category of "compassionate" homicide that would remove the killing of a person with a serious disability or illness from the definition of murder, or at least significantly reduce or eliminate the mandatory penalty for committing such crimes.
- Society in general attributes negative characteristics to persons with disabilities. Their lives are regarded as having less value, both to themselves and to the society around them, than the lives of individuals who do not have disabilities. As a consequence, there is less resistance to any practice that ends their lives prematurely. The legalized practice of assistance in dying could result in a disproportionate number of persons with disabilities being put to death, either voluntarily or otherwise.
- Examples are provided where parents have recently murdered or attempted to murder their children, and where they have been spared the normal penalty required by the law, or where there has been vigourous campaigning on behalf of the parents that their sentences should be significantly less than the law requires. Making such parents pay the penalty they undoubtedly would have had to pay had their children not been disabled has been branded by some (but not by the courts) as "cruel and unusual punishment", and as such contrary to s. 12 of the Canadian Charter of Rights and Freedoms.
- The notion that a person with a disability has an unacceptably poor "quality of life" influences people's judgment as to whether such a person ought to receive needed medical care. "Do Not Resuscitate" orders are often made, not because a person's medical condition is untreatable, but because their disability is regarded as having made their life of negative value.
- The current law in Canada pertaining to assistance in dying is reviewed. The Criminal Code of Canada prohibits both active euthanasia (i.e., using lethal measures with the intention of causing another person's death) and assisted suicide (i.e., providing the means and instructions whereby an individual may end his or her own life). The actual enforcement of these criminal sanctions, however, has not been consistent, perhaps because prosecution of a health care practitioner may discourage other professionals from offering adequate pain control and/or from terminating futile treatment.
- Canada's Constitution, in s. 7 of the Canadian Charter of Rights and Freedoms, provides some assurance that both the right not to have one's life artificially shortened (the right to life and the right to security of the person) and the right to decide the time of one's own death (the right to liberty) will be respected. Section 15 of the Charter guarantees to everyone the right to equality before and under the law and the right to the equal protection and benefit of the law. Constitutional guarantees, however, are only binding on legislatures and those who act with the authority of government, and not on private decision makers or health practitioners.
- Canadian case law requires that the wishes of a mentally capable person to forego life-sustaining medical treatment must be respected. Administering drugs for the purpose of controlling pain, particularly in a case where death is imminent, is permissible, even if it is likely that the type and amount of medication required to do so might hasten the patient's death, so long as the intention is to relieve pain, rather than to cause death.
- The courts have shown willingness to intervene in order to prevent a surrogate decision in favour of the death of a child with a disability whose physical condition was treatable. Similarly, the case of Sue Rodriguez, who unsuccessfully challenged the law against assisting suicide, demonstrates the tendency of the courts to err on the side of preserving life.
- In the latter half of the decade of the 1990's, a Senate Committee on Euthanasia and Assisted Suicide examined a full range of issues relating to Canadian law and policy on end-of-life decisions. In its 1995 report, "Of Life and Death", the Senate Committee affirmed the existing Criminal Code provisions against all forms of euthanasia and assisted suicide. The Committee also stressed the importance of developing and providing improved palliative care and more effective means of pain control. The Committee called for amendments to the Criminal Code to clarify when it is permissible to provide pain relief that may also have the effect of shortening a patient's life, and when the withholding or withdrawal of life-sustaining treatment is acceptable.
- A minority of Senators on the Senate Committee on Euthanasia and Assisted Suicide wanted the Criminal Code to be amended to permit assisted suicide and to reduce the severity of penalties for "voluntary euthanasia". These relaxations of the current law, according to the minority, would only be permissible if there were procedural safeguards including review of each case both before and after the death of the individual. Several witnesses who appeared before the Senate Committee expressed serious misgivings about the possibility of maintaining genuine voluntariness in any system that permits euthanasia or assisted suicide. A majority of the Committee favoured a less severe penalty for homicide in which there is a clear element of compassion.
- Extensive safeguards against the abuse of legally permissible assistance in dying were articulated by some witnesses before the Senate Committee, and also in the minority opinions of the Chief Justices of British Columbia and of Canada in the two unsuccessful appeals by Sue Rodriguez to gain legal approval of her assisted suicide plans. In each case these recommendations included both a before-the-fact hearing process and an after-the-fact review of the appropriateness of the decision in favour of death.
- A Senate Subcommittee appointed in 1999 reviewed the developments in the field since the original 1995 report, "Of Life and Death". The Subcommittee tabled a report entitled "Quality End-of-Life Care: The Right of Every Canadian" in June, 2000. The distinctions between the titles given to the respective Senate reports are significant, although the Subcommittee restricted itself to a review of progress made with respect to the unanimous recommendations of the earlier Senate Committee on Euthanasia and Assisted Suicide, which did not include the legalization of either euthanasia or assisted suicide. The Subcommittee expressed concern that very few advances had been made in the intervening five years in the end-of-life practices of palliative care, pain control, sedation, the withholding or withdrawal of life-sustaining treatment, and advance directives.
- The Senate Subcommittee reported in 2000 that only about five percent of dying Canadians receive appropriate palliative care. They singled out several elements of palliative care and several subpopulations of Canadians, including persons with disabilities, in which emerging valuable principles and practices in end-of-life care were particularly neglected. The Subcommittee focussed on the social context in which death occurs as having at least as significant an impact as the medical context. The social context of caring and love, if it exists at all, is inevitably one in which close family members and friends desire that the dying person's symptoms and pain be relieved by whatever reasonable means are available other than causing the person's death.
- Research findings reported to the 1999-2000 Senate Subcommittee included the information that appropriate and effective pain control hardly ever has the consequence of hastening a patient's death, and that treatable clinical depression often is associated with expressions of a desire to have one's life ended unnecessarily by artificial means.
- There have been some recent proposals, including private members' bills, to legislate clearer guidelines for end-of-life care. Bill S-2, introduced in the Canadian Senate in 1999, would have essentially codified law that is already in effect, although it attempted to go a step further and identified "artificial hydration and nutrition" as "life-sustaining medical treatment" which could be withdrawn lawfully on the consent of a family member.
- A series of court cases in the United States during the 1980's focussed on individuals with disabilities who sought the endorsement of the courts for their wishes to die because they said that their disabilities made their lives intolerable. The courts generally allowed the petitioners the same right to refuse treatment that persons without disabilities have, although there was little attention paid to the ways in which society's failure to provide needed material, social and health-related supports contributed to the circumstances leading the persons with disabilities to seek passive euthanasia.
- In two other cases in 1997 the U.S. Supreme Court upheld the validity of State legislation banning physician-assisted suicide. The Court ruled that such laws are intended for the protection of vulnerable individuals "whose autonomy and well-being are already compromised", including the poor, the elderly and persons with disabilities, against "the real risk of subtle coercion and undue influence in end of life decisions". Suicide prevention was chosen in preference to suicide facilitation. More recently the Alaska Supreme Court rendered a similar decision, rejecting the argument that a decision to end one's own life is a private matter. It becomes a public matter when approving the practice would put other vulnerable persons at risk. The judge wrote that a "disabled person's suicidal impulses should be interrupted and treated the same way as anyone else's".
- The State of Oregon in 1997 became the first and so far the only State in the U.S.A. to enact legislation, the Death with Dignity Act, permitting physician-assisted suicide for those who are terminally ill, likely to die within six months, and who freely choose to end their lives. During the first two years after enactment of the legislation, fewer than one percent of cancer deaths, the largest category of terminal diseases, were listed as assisted suicides. The numbers exercising their right to end their own lives with the assistance of a doctor actually decreased in 2001. Only the patient, two physicians and two witnesses are required by the law to have knowledge of the patient's intention to end his or her life before the fact. Some researchers maintain that there is reason to believe that many who chose assisted suicide under Oregon's law are motivated by depression, despite the provision in the statute that patients requesting assisted death are to be referred to a counsellor to determine whether they may be making an "impaired judgment". The procedure has also been criticized for failing to demonstrate that palliative care interventions are available as an alternative to consensual death.
- In 2000 the U.S. House of Representatives passed the Pain Relief Promotion Act, which had the stated purpose of promoting pain management and palliative care without permitting assisted suicide and euthanasia. The clear intention of the Bill was to render the Oregon Death with Dignity Act inoperative. It has never come to a vote in the U.S. Senate. With the change of the United States federal administration early in 2001, Attorney General John Ashcroft, reversing the instructions of the previous Attorney General Janet Reno, ordered that the U.S. Controlled Substances Act should be interpreted in such a way as to make it illegal for medical practitioners to prescribe lethal drugs for the purposes of assisting suicide or euthanasia. That order was struck down by the court, but is currently under appeal.
- The Netherlands has taken the lead in legalizing physician-assisted death on a national scale, having effectively tolerated it for more than twenty years. Formal passage of legislation expressly permitting it took place in April, 2001. Under the legislation, no evidence of terminal illness is required, but the physician is expected to be of the opinion that a candidate for assistance in dying is facing "unremitting and unbearable suffering", for which there is no reasonable alternative solution. Active euthanasia by lethal injection has historically accounted for many more assisted deaths in the Netherlands than has assisted suicide. There is also evidence that a significant number of such deaths (in the order of 1,000 cases per year) take place without the personal consent of the individual, and that more than half of all cases of assisted death are not reported at all.
- Some investigators maintain that the incidence of assisted death is not actually lower in countries where the law prohibits it, but that in those countries it takes place secretly. One Australian study concluded that "intentionally accelerated deaths" in that country happen almost twice as frequently as in the Netherlands. Canada, too, is alleged to have an "underground assisted death movement" that has grown particularly towards the end of the twentieth century with the emergence of AIDS as a cause of terminal illnesses.
- One Australian jurisdiction, the Northern Territory, briefly enacted legislation permitting assisted death in 1996, but the National Senate overturned the law less than one year later. Other states where assisted death continues to be formally condoned include Colombia, Switzerland and Belgium. Draft legislation to remove any criminal sanction against assisted death exists in some of these countries, and also in Scotland, South Africa, and some U.S. States.
- Groups favouring euthanasia and/or assisted suicide continue to propose changes to the law which would permit such practices where they are now legally prohibited. A "Model State Act to Authorize and Regulate Physician-Assisted Suicide" has been proposed by representatives of the pro-euthanasia Hemlock Society. The preamble to the draft legislation gives as its rationale the fact that effective therapeutic or palliative care is for some people "impracticable because the patient lacks the resources or health insurance necessary to pay for them". It is submitted that this attitude is especially dangerous to persons with disabilities, who are the most likely to be without the necessary resources, and for whom some may regard the expenditure of health care resources as a waste, since they will not "cure" the individual's disability, even though they may prolong his or her life.
- Any system that permits euthanasia or assisted suicide, but that provides minimal legislated safeguards, will leave many vulnerable persons at risk of losing either their lives unnecessarily, or their autonomy over personal life-and-death decisions, or both. Treatable depression is often regarded as a justification for a decision to end a person's life. However, the risks people with disabilities seem to face, according to anecdotal reports, are not greatly different in jurisdictions that have made assisted death legal, as compared to what they are in other jurisdictions where strict prohibitions remain in effect. The devaluation of the lives of persons with disabilities is a universal reality, and often leads to preventable death, even if not planned and deliberate death.
- "Do not resuscitate" orders are often entered in patient charts, not because an attempt to resuscitate the person would be futile, but because the individual's life is negatively valued because of disability. There is a reluctance to resort to professional discipline or criminal prosecution in cases where the life that is taken is that of a person with a disability. These observations do not reduce the concern over the prospect of legalization of assisted death as much as they underline the critical need for improved support services life-long, strong individual and systemic advocacy, and appropriate palliative care as death draws near.
- Persons with disabilities have been shown to place just as great a value on their lives as do persons without disabilities. The critical factor in safeguarding the lives of persons with disabilities is to develop in society a true awareness of the value of every human life. Only when this happens can there be any real assurance that personal supports and protections against discrimination on the grounds of disability will be sufficient to ensure that the lives of persons with disabilities do not become intolerable. The slogan, "death with dignity" is a cruel hoax if there is not comparable commitment to "life with dignity" for those who have disabilities. When death becomes imminent and inevitable, the priority ought to be to ensure that as long as any individual's life goes on it remains a life of acceptable quality and comfort. The two recent reports emanating form the Canadian Senate have asserted that priority as a necessary national commitment.
- If patients are either over-treated or under-treated because their physicians are fearful for their own protection from prosecution or professional discipline, steps must be taken to bring greater clarity to the law and/or to people's understanding of the law, and greater consistency in the law's enforcement. Mandatory severe punishment does not adequately deter doctors from killing their patients, in part because it deters prosecutors from charging them and juries from convicting them. On the other hand, bringing in provisions for lenient penalties under the guise of "compassionate homicide" would amount to an invitation to inflict death on vulnerable persons by making the protection of health care practitioners more of a priority than the protection of the lives of their patients.
- Those in Canada who have favoured some relaxation of the laws prohibiting euthanasia and assisted suicide have tended to link their arguments with recommendations for the establishment of a serious set of procedural safeguards to try to prevent abuse. This is true of judges who wrote minority judgments in the Rodriguez case and minority members of the Senate Committee. Their proposed safeguards have often taken the form of an application to the court or to a quasi-judicial tribunal for approval before assistance in dying is permissible. One variation would have the decision-making body assisted by a cross-disciplinary "advisory panel". These precautions stand in sharp contrast to the practices that are currently allowed by legislation in the Netherlands and Oregon, where there is no provision for independent assessment of whether a request for assistance in dying ought to be granted, but rather a loose requirement that the death be reported after it has taken place.
- In addition to the role of the court or a quasi-judicial hearing panel to authorize legalized assistance in dying, there would be a need for publicly funded advocacy on behalf of the individuals who seek to have their lives ended, in order to make sure that they understand all of the options available to them, and that their request has not been motivated by some form of manipulation by other persons. One of the most difficult criteria to satisfy is that persons with disabilities who are deemed to be candidates for assistance in dying can choose that option without coercion or undue influence.
- Next to the determination that a choice of assistance in dying is without doubt the free and voluntary decision of the patient, the other most essential criterion is that every reasonable avenue has been fully explored that would make dying no longer the most attractive prospect, either for the person or those near them. This must include readily available pain relief and all aspects of palliative care, as well as an examination of non-medical issues that impact on the individual's will to live.
- For persons with disabilities, the "mercy" in what is popularly called "mercy killing" is far too often understood in terms of ending a life that is inherently of negative value to the individual, to their families and to society, rather than as a response to pain and suffering experienced by the individual that cannot otherwise be relieved. Even in Canada, where the law officially continues to uphold the traditional uncompromising respect for human life, safeguards against resorting to assisted death are seriously wanting. Until it can be convincingly demonstrated that all Canadians enjoy full equality and security of the person, regardless of disability, as guaranteed by the Charter of Rights and Freedoms, then any steps toward legalized assistance in dying should be resisted.
LEGALIZING PHYSICIAN-ASSISTED DEATH:
CAN SAFEGUARDS PROTECT THE INTERESTS OF VULNERABLE PERSONS?
*
I. INTRODUCTION
The issues surrounding the legalization of euthanasia and physician-assisted suicide are preoccupying legislators, the judiciary, health care practitioners, legal scholars, ethicists and the general public to an ever-increasing degree around the world. Precedents have been established in some jurisdictions where euthanasia and/or physician-assisted suicide have been legalized. Changes to the law are also currently under serious consideration in many other places.
The movement towards the removal of legal penalties for physicians who hasten the death of their patients poses several problems for persons who are vulnerable because of disability or advancing age. These problems exist in two interrelated areas:
- the threat of being put to death against one's wishes, and
- the threat of losing one=s control over the most significant decision affecting one=s life that it is possible to make — the decision to bring it to an end before death occurs naturally.
In the event that Canadian law may, at some point in the future, be amended to permit physician-assisted death, the Council of Canadians with Disabilities (CCD) wants to have a thorough understanding of what safeguards have been proposed or might be proposed, and of the adequacy or inadequacy of such measures as reliable protections of the lives and liberties of vulnerable persons.1
The paper will first consider why physician-assisted death poses a special threat to persons with disabilities. It will then examine current Canadian statute law, both criminal and civil, the Constitution, case law, and prosecutorial practice in order to identify the existing baseline of what is and is not permissible, the extent to which prohibitions are enforced, and what protections they provide of the lives and freedoms of vulnerable persons in this country. The paper will then turn to developments in other jurisdictions where restrictions on physician-assisted death have been relaxed, or where attempts have been made to do so. Particular attention will be paid to the elements of such laws and practices that can be construed as safeguards, either against abuses generally, or against interference with the life, liberty and security interests of vulnerable persons.
The proposition that our society ought to permit doctors to act as agents of death in certain situations presents frightening concerns about both personal safety and autonomy for persons with disabilities. Any discussion of safeguards must pay full attention to both types of concerns. In matters that are not obviously life and death issues, our society has a history of presenting persons with disabilities with the choice between deciding for themselves, which is supposed to be risky, or having non-disabled persons make decisions for them, which is supposed to be safe. There is also a frequent phenomenon in which persons are supposedly deciding for themselves, but in fact decisions are being made for them. When the issue is the decision to live or to die, this may be the most difficult circumstance against which to develop safeguards.
A related focus of debate which this paper will touch upon is whether there ought to be a separate category of homicide in Canada, often referred to as "compassionate homicide" or "mercy killing". It is conceivable that Parliament may, as was recommended in 1995 by the Special Senate Committee on Euthanasia and Assisted Suicide,2 adopt this as an interim amendment to the Criminal Code, rather than moving directly to specific physician-assisted death legislation. At present the Criminal Code classifies murder as "first degree murder" if it is "planned and deliberate", if the victim is a peace officer or prison employee "acting in the course of his duties", or if the murder takes place while the accused person was "committing or attempting to commit" certain other serious offences. All other murder is second degree murder.3 Some have been urging in recent years that anyone who kills another person with the intention of ending their pain and suffering should not be subject to the life sentence and minimum periods of parole ineligibility that are at present mandatory for those convicted of first and second degree murder. The event that has brought this issue into sharp focus in Canada is the 1993 murder of Tracy Latimer by her father, Robert Latimer, whose appeal was heard by the Supreme Court of Canada in June, 2000, and denied in a decision released in January, 2001. This paper will examine the Latimer case in some detail below.
It is not the purpose of this paper to enter into the broad debate about euthanasia and assisted suicide. For the most part, that debate is conducted without much reference to the particular concerns of persons whose lives and liberties might be jeopardized, if such practices are legalized, because they have disabilities. However, it is obvious that, to the extent that potential safeguards appear inadequate to protect the interests of vulnerable persons, the paper will oppose any relaxation of existing law that prohibits physician-assisted death.4
Canadian law now prohibits both "euthanasia" and "assisted suicide". Euthanasia (literally "good death") is generally understood to mean the intentional taking of one person's life by another for the purpose of relieving the first person of the anguish of uncontrollable pain or prolonged dying. The expression "active euthanasia" is often used, signifying that death was brought about by the commission of a lethal act, rather than by the omission of some potentially life-sustaining intervention, which is correspondingly referred to as "passive euthanasia".
The Criminal Code of Canada does not distinguish active euthanasia from homicide, which is defined as "directly or indirectly, by any means, (causing) the death of a human being".5 Assisted suicide means providing a person with the means or assistance necessary in order to cause his or her own death. Both "counselling" and "aiding and abetting" a person to commit suicide, whether the person actually commits suicide or not, are also prohibited by the Criminal Code.6
Canadian law does not, where consent has been properly given or refused, prohibit the withholding or withdrawal of treatment without which death will likely or inevitably occur. In cases of so-called "passive euthanasia", the law regards death as a consequence of allowing the dying process to take its course without intervention or "causation" by another person. This may be a form of legal fiction, however, in that certain forms of termination of treatment ("pulling the plug" in colloquial terms) clearly do cause death, and would therefore seem to fall within the definition of homicide in s. 222 of the Criminal Code.
In fact, however, the law labels as assaults any interventions upon his or her person to which a mentally capable individual refuses or withdraws consent, even if the consequence is likely or certain to be death.7 Such refusal or withdrawal of consent can be that of the individual at the time the intervention is proposed, or by means of an advance directive, either spoken or written. When written, such advance directives are often referred to as "living wills". In some circumstances, which will be reviewed below, substitute decision makers may make the decision on their own to forego treatment on behalf of a mentally incapable individual, without any advance directive.
The distinction between killing and allowing to die in the health care context has been stressed by some commentators and minimized by others.8 This is also a debate that will not occupy the present study, other than to note the obviously crucial fact that active euthanasia and assisted suicide are violations of existing law in Canada, and that withholding or withdrawing treatment (if in accordance with the relevant principles governing health care decisions) is not. This distinction provides an opportunity to consider whether any safeguards that serve to protect vulnerable persons from unwarranted passive euthanasia may have counterparts that would protect people from abuse if the law were to be changed in order to permit active euthanasia or physician-assisted suicide.
It is also generally the case that the law permits the use of drugs for the control of pain or other distress, particularly where the patient is clearly dying, even if it is likely that such drugs will also serve to shorten the person's life. In such circumstances, the lawfulness of giving the drug depends on the intention being the relief of suffering, rather than to cause death. Intention can usually be inferred from the type and quantity of a drug that is given.
The title of this study includes the phrase "physician-assisted death" on the understanding that any amendments to the law that may take place in Canada will probably follow the precedents established in other countries, where the agent of death is almost always to be a member of the medical profession. In spite of the fact that physicians generally oppose the enactment of laws that would bestow such responsibility on them, it appears to be taken for granted that only doctors should be permitted to take measures to end a person's life in certain prescribed circumstances without incurring criminal liability. This assumption has been questioned, and may well deserve critical examination.9
II. INDICATORS OF THE DEVALUATION OF THE LIVES AND FREEDOMS OF PERSONS WITH DISABILITIES
On November 30, 1999 a mother in Ontario who had tried to kill her six-year-old daughter who has cerebral palsy by administering an over-dose of medication was given a two year conditional sentence, which she will be permitted to serve in the community. The next day the Toronto Star printed a story under the headline "No jail for failed mercy killer". Without going into the rationale for the sentence or commenting on its appropriateness, the striking thing about the story was the headline. No facts were reported suggesting that the girl was suffering any pain or that she was near death from an incurable illness. In fact, her ability to withstand the assault on her life suggests that she was both healthy and had a strong will to live. The headline would seem to have been written on the basis of an assumption that causing the death of any individual who has a disability is an act of "mercy". That is an assumption made by a very sizeable proportion of people in Canadian society and in other countries as well.
Another act of parental homicide, in this case successful, was the killing in Saskatchewan of Tracy Latimer by her father, Robert Latimer, in 1993. Tracy, who also had cerebral palsy, did apparently experience a great deal of pain from time to time as a result of her condition. Tracy also experienced many positive things. She was scheduled to have surgery which would very likely have relieved her pain to a considerable degree. Robert Latimer decided to intervene before Tracy could have the operation by placing her in the cab of his truck and piping exhaust gases through a window until she died of carbon monoxide poisoning.10
Notwithstanding the fact that the killing of Tracy Latimer corresponded to the Criminal Code of Canada's definition of first degree murder ("Murder is first degree murder when it is planned and deliberate"11), Robert Latimer was charged with and convicted of second degree murder. The reduction of Robert Latimer's charge from first to second degree murder is significant. When capital punishment was abolished in Canada in 1976, the Criminal Code was amended to provide a mandatory life sentence for murder, either of the first or second degree. These amendments also provided that a person convicted of first degree murder is not eligible for parole until twenty-five years of the life sentence have been served, and that those convicted of second degree murder are ineligible for parole until they have served ten years of their sentence.12
In spite of the leniency exhibited by the reduction of Robert Latimer's minimum period of potential incarceration by sixty percent, public opinion in Canada, and the opinions of two out of the eight Saskatchewan judges who addressed this issue at both the trial and the appeal levels, have favoured a further substantial reduction in the amount of time he ought to be required to spend in prison. Legal and ethical scholars have renewed their urging that a third degree of murder be recognized in Canada — "compassionate homicide" — for which there would be no mandatory minimum period of incarceration.
The judge at Latimer's second trial (the first having been declared a mistrial because the police had interrogated potential jurors, at the request of the Crown Attorney, about their attitudes towards persons with disabilities) granted a constitutional exemption from the ten year no-parole provision of the Criminal Code on the grounds that in his case it would constitute cruel and unusual punishment, and so violate his rights under s.12 of the Canadian Charter of Rights and Freedoms.13 The trial judge imposed a sentence of one year in prison, to be followed by an additional year of confinement to his farm. The Saskatchewan Court of Appeal upheld Latimer's conviction and overturned the trial judge's constitutional exemption, disallowing the reduced sentence.
The Supreme Court of Canada granted Latimer leave to appeal both his conviction and sentence, but dismissed both appeals on January 18, 2001. The unanimous opinion of the Court was that
... denunciation becomes much more important in the consideration of sentencing in cases where... like-minded individuals may well be deterred by severe sentences.... This is particularly so where the victim is a vulnerable person with respect to age, disability, or other similar factors.14
Both before and after the Latimer case was finally decided in the Supreme Court of Canada, public opinion has tended to oppose the imposition of the minimum sentence the law requires in a case of second degree murder. A campaign continues to persuade the federal Cabinet to exercise the Royal Prerogative of mercy, and release Robert Latimer as soon as possible.
In October, 2000, the Provincial Museum of Alberta opened an exhibit entitled "Anno Domini" to mark the 2000th anniversary of the life of Jesus Christ. Part of that exhibit included written and videotaped references to Robert Latimer's murder of his daughter as an example of the contemporary meaning of Jesus' teaching as recorded in the Gospel of Matthew, "Blessed are the merciful".15 Throughout the court process, the main theme of Robert Latimer's defence was that his act was entirely motivated by his "merciful" regard for his daughter.
These examples of parents having killed or attempted to kill their children with disabilities (there have been several more such instances in Canada in recent years) serve to illustrate that the lives of persons with disabilities are very widely regarded by the general public, and also by family members and by persons in a position to influence public policy, judicial decisions and legislative change, as being unworthy of the legal protections that are ordinarily available to those who do not have disabilities. The words of the Factum of the Intervener, COPOH (Coalition of Provincial Organizations of the Handicapped), now the Council of Canadians with Disabilities (CCD), in Sue Rodriguez's 1993 appeal to the Supreme Court to authorize her doctor-assisted suicide, express this reality very well:
Both historically and to the present day the lives and freedoms of persons with disabilities have been threatened and, in some cases, eliminated by the insensitivity, ignorance and hostility of those who believe that the lives of disabled people are somehow of less value or quality than those of other people.
These kinds of attitudes, in their most extreme form, resulted in programs in Nazi Germany directed towards the sterilization and mass murders of hundreds of thousands of persons with disabilities. Under Nazi ideology, it was seen as important for the better public good that precious resources not be wasted on unworthy lives. Programs to kill people with disabilities were described as "the destruction of life devoid of value", "the destruction of useless eaters", and "help for the dying".16
Six years later CCD intervened in the 1999 Ontario appeal of R. v. Genereux.17 Dr. Genereux pleaded guilty to aiding and abetting suicide after prescribing lethal quantities of a barbiturate to two men who were HIV-positive. One of the men died after taking the drug and the other survived after attempting to commit suicide. Once again, CCD placed before the Court of Appeal for Ontario a compelling summary of the situation of persons with disabilities in Canada:
(a) Vulnerability of People with Disabilities
4. The history of disabled persons in Canada is a history of marginalization, exclusion and social devaluation. At the heart of this history is the perception of disabled persons as abnormal, or as existing in tragic and unbearable circumstances. As a consequence of that perception, disabled persons have been exposed to victimization and discrimination.
5. Society attributes negative characteristics to disabled persons. These negative attitudes are reinforced by actions, attitudes and beliefs, which often characterize disabled persons as being less than human. The perception that disabled persons have lives that are of less value than the lives of individuals without disabilities reinforces rationalizations for treating disabled persons prejudicially.18
It must not be forgotten that the Nazi-era holocaust was initially focussed on the extermination of persons with disabilities. It is generally estimated that at least a quarter of a million persons perished in this program, in which Hitler had the full co-operation and assistance of many members of the medical profession.19 As in the case of many crimes against humanity committed during that period, very few people have ever faced prosecution, or else the delay in prosecuting such gross offenders has only magnified the scandal.20
These episodes from more than half a century ago are still reflected in the attitudes and practices of some members of the medical community today. According to Hugh Scher, Chair of the Human Rights Committee of the Council of Canadians with Disabilities, often "when people with disabilities go in for a tonsillectomy one of the first questions they are asked is whether they want a do-not-resuscitate order put on their chart".21
If the movement to legalize physician-assisted death gains momentum at the dawn of the twenty-first century, there is every reason to expect that a disproportionate number of those who will be "assisted", both within the terms of the law and otherwise, will be persons with disabilities.
III. WHAT NEEDS TO BE GUARDED AGAINST?
History tells us that the primary threat to persons with disabilities of legalizing assisted death will be that many will lose their lives involuntarily. A secondary and related threat is that they will lose their right to self-determination. It is difficult to conceive of safeguards that will deal with both kinds of threat. If the safeguards are designed primarily to prevent wrongful deaths, specifically of persons who are vulnerable, then it is likely that such persons will have more limited access to the freedom to choose death that the more relaxed laws will afford to other people. This is a form of discrimination which was recognized as such by both the five-member majority and two of the four-member minority in the Supreme Court of Canada in the Rodriguez case22 as a violation of the constitutional right to equality which s. 15(1) of the Canadian Charter of Rights and Freedoms explicitly grants to persons with disabilities.
Section 7 of the Charter begins with the words, "Everyone has the right to life, liberty and security of the person". Such a guarantee ought to be expressed in legislation and public policies that will protect the right to life itself, and the liberty to make of one's life what one chooses. Whether this includes the right to choose the time and means of ending one's life is a question that must be faced. This study will assume that, for persons with disabilities, the more serious threat is that of unwanted death, and that the threat of unwarranted loss of personal autonomy is an important but secondary concern. If people lose the right to choose death on their own terms, at least they can continue to fight for that right.
A. Wrongful death
The law, both in Canada and elsewhere, has a long history of opposing any action that will end a person's life by "unnatural" means.21 Even suicide itself was once considered a crime, and attempted suicide was treated as such until relatively recently. The Criminal Code of Canada not only prohibits homicide and aiding and abetting suicide. It also declares that
No person is entitled to consent to have death inflicted on him, and such consent does not affect the criminal responsibility of any person by whom death may be inflicted on the person by whom consent is given.22
The Supreme Courts of both Canada and the United States have ruled that there is no constitutional right to physician-assisted death in either country.23 Sue Rodriguez, who had amyotrophic lateral sclerosis, asked the Court to order that the Criminal Code prohibition of assisted suicide was unconstitutional in her case because it discriminated against her on grounds of disability. The Court, in a 5-4 split decision, denied her request. The U.S. Supreme Court cases held that statutory prohibitions of physician-assisted suicide in New York and Washington States were constitutionally valid.
The medical profession has historically been as opposed to causing death as has the law.
The Hippocratic Oath (400 b.c.e.) includes the following vow:
To please no one will I prescribe a deadly drug nor give advice which may cause his death.
Historically, however, where an individual was perceived to have a significant disability, both law and medicine have tended to make exceptions to their own life-preserving rules, or at least to be very uncertain about their application. The Canadian case of Stephen Dawson24 illustrates this ambivalence. Stephen was a seven-year-old boy who had a combination of physical and intellectual disabilities. His parents had placed him in a facility when he was two. He had hydrocephaly as a consequence of meningitis which he contracted as a baby. In 1983 the shunt which had been installed to drain cerebrospinal fluid from his head became blocked. Fluid was building up inside his cranium, causing great discomfort and posing a threat to his life. His parents were asked to consent to a procedure known as a "revision" of the shunt. When they refused their consent, stating that they preferred that he should die, the responsible child welfare authorities petitioned the Provincial Court for an interim custody order for the purpose of authorizing the surgery which Stephen required. The Court dismissed the application.
The next day an application for judicial review of the Provincial Court decision was commenced in the Supreme Court of British Columbia. Some of the witnesses who had been heard in the Provincial Court testified again, but there were also new witnesses who provided a much more positive view of Stephen's life. Justice Lloyd MacKenzie of the B.C. Supreme Court ruled that Stephen was legally entitled to the surgery that would save his life. He wrote that, if he had declined to order that Stephen be treated,
This would mean regarding the life of a handicapped child as not only less valuable than the life of a normal child, but so much less valuable that it is not worth preserving. I tremble at contemplating the consequences if the lives of disabled persons are dependent upon such judgments.25
In spite of this landmark decision, it remains a reality that for many members of our society (and of other societies around the world and down through history) the lives of persons with disabilities continue to be regarded as less valuable than the lives of other persons. Furthermore, this assessment is often reflected in the opinions of academics who hold themselves out as advisors to those who make public policy. For example, University of Victoria ethicist, Professor E.-H. Kluge, described the outcome of the Dawson case as having inflicted upon Stephen "the injury of continued existence".26 The central flaw in this perception is that the "injury" is identified with the disability — not the life threatening condition. Because the disability is thought not to be amenable to any significant change, the conclusion is to relieve the "injury" by ending the person's existence. Fortunately for Stephen Dawson, Justice MacKenzie perceived that his only real "injury" was the malfunctioning shunt, which could be repaired.
How often, when a person with a disability has a life threatening physical ailment, do people (including health care professionals) become fixated on the disability as the presenting problem? How often is the notion of an unacceptably poor "quality of life" used as an excuse to deprive a person of life by refusing to treat a medical problem? In Stephen Dawson's case, the increased pressure of the cerebrospinal fluid building up in his head clearly did interfere with his quality of life, but the Provincial Court Judge ignored that fact, and determined that his quality of life, even apart from the critical medical problem, was insufficient to warrant the intervention he required.
How often, when a person's disability is such that he or she has difficulty communicating his or her wishes, do people (including health care professionals) latch onto the failure to provide valid consent to treatment as the presenting problem, even when the condition that needs treatment easily qualifies as an emergency, in which case the law does not require the obtaining of consent?27 Conversely, how often do health care professionals take "No" as an answer to their question, "Do you want to have this operation?" when they have not taken the trouble to make sure that a person with an intellectual disability is adequately informed as to why the operation is needed and what the consequences will be if it is not performed? If informed consent cannot be obtained from the individual, do health care professionals turn in a timely way to the person or persons authorized by law to give substitute consent for the individual?
How often, when a person has a disability that involves depression, perhaps to the point of suicidal despair, have such persons been denied the supports and treatment that could have restored their desire to live? If assisted death becomes more easily accessible, will it become a fatal error to express the wish to die? Will offers of help in coping with depression come to be regarded as an intrusion into the privacy and autonomy of an individual who has opted for death as a socially and legally approved solution to his or her despair?
The answers to these questions are not always clear, but they illustrate the kinds of situations in which the lives of persons with disabilities are put needlessly at risk because they have disabilities, rather than because of the inherent seriousness of their medical conditions. It is clear that wrongful death is a consequence that must be guarded against by whatever means are possible, even with the existing legal prohibitions of homicide and assisted suicide in place. If those prohibitions are to be relaxed, then the prospect of unwanted death being imposed on persons with disabilities will become considerable more likely, and new safeguards must be in place that will replace the present one's to as full an extent as is possible. The risk is that relaxing the legal restrictions will lend greater acceptability to practices of denying life-sustaining treatment that some regard as all too acceptable already. Ideally, if new safeguards are to be enacted, they should be such that will make persons with disabilities safer from unwanted death than they are now — because they are not very safe as things now stand.
B. Loss of personal autonomy
The arguments in favour of legalizing physician-assisted death are presented primarily in terms of the need people feel to be able to exercise personal control over the time and means of their dying, once death becomes both imminent and inevitable, and preferable (in their judgment) to continuing to live. Sue Rodriguez's case was based on the contention that she needed to be as free as a person without a disability would be to make the decision that the time had come to die. She anticipated that she might live beyond the point at which she could put that decision into effect without the assistance of another person, notably a doctor.
This principle of self-determination is well established where the decision is to reject measures to prolong one's life — in other words to refuse life-sustaining treatment. Personal autonomy in such cases can be exercised directly by the individual, or through an advance directive ("living will") which it becomes the legal responsibility of a substitute decision maker to carry out.
If the law were to be changed to legalize physician-assisted suicide or euthanasia by active means (i.e. taking or administering lethal drugs) presumably the rules now in effect for refusing life-sustaining treatment would continue to apply. Essentially, those rules are very simple: the individual (or the substitute decision maker) must be capable of making an informed decision, and the decision must be both freely made and based on adequate information. It can be anticipated that additional rules would apply where active means were to be used to hasten the person's death, such as concurring opinions of other health care professionals, an established waiting period before the decision can be carried out, and possibly the prior approval of a court or other tribunal.
For our present purposes, however, the key question is whether a person with a disability would be accorded the same degree of freedom to make up his or her own mind about the method and timing of dying. Those with more severe cognitive impairments would probably be deemed incapable of making such decisions at all, and so the decider would have to be someone with authority to make decisions for them. Choosing death by any means, active or passive, at the determination of a third party, will always be problematic. Safeguards particularly designed for such situations will be examined below. Some already exist in Canadian law with respect to decisions to forego treatment.
Another important aspect of personal autonomy is whether and how it can be protected from subtle or not-so-subtle pressures from other persons. Whether there are conflicting interests or not, persons with disabilities, especially cognitive impairment, ordinarily experience considerable difficulty in exercising an unfettered right of self-determination in the entire gamut of personal decision making. Where the decision is when and how to die, such interference can be expected to be even more powerful and pervasive. Influences on one's personal autonomy will be based on any number of factors: the burden, both in terms of personal energies and financial costs, that family members experience in providing care for the individual, the anticipated advantage of dividing up an estate, or the simple "how we hate to see you suffer so" approach.
Catherine Frazee has pointed out that "relief from the psychic pain and the discomfort that is generally felt by the non-disabled in the presence of disability" is another personal interest that can influence choices made by individuals who have legal or de facto control over life and death decisions affecting persons with disabilities.28
Most crucial of all the possible motivations for such interference is the underlying belief that the person's life is worth less to him or her than the lives of persons who do not have disabilities are to them. Conversely, some may experience pressures not to decide to die sooner rather than later. These could be pressures based on another person's moral values, personal need for companionship, or the desire to be needed by a vulnerable person.
This is not to say that there is no place for any attempt by those who value the life of the individual to try to show the person that life is worth living after all. The key element is that all such efforts must be infused with a real belief in the value of the person and a willingness to speak and act in ways that help the person to appreciate his or her own value, and to discover that he or she is valued by others.
The most serious threat to personal autonomy represented in the anticipated relaxation of laws and moral values that presently favour life will perhaps be the development of a culture in which death before nature takes its course becomes a societal ideal, to which all members of the society will be expected to conform. It is extremely difficult even to contemplate how safeguards can be fashioned against such an all-pervasive shift in values.
The Canadian Medical Association has adopted an interesting argument in its opposition to the legalizing of physician-assisted death.
Consideration should be given to whether any proposed legislation can restrict [active] euthanasia and assisted suicide to the indications intended. If [active] euthanasia or assisted suicide or both are permitted for competent, suffering, terminally ill patients, there may be legal challenges, based on the Canadian Charter of Rights and Freedoms, to extend these practices to others who are not competent, suffering or terminally ill. Such extension is the "slippery slope" that many fear.29
According to this approach, some groups would be put at risk of unwanted death because certain members of one or more of such groups would mount a court challenge against any physician-assisted death provision that deprived them of the equal opportunity to take advantage of the permissive law. This is not a particularly compelling argument, but it does suggest that safeguards against death and safeguards against loss of liberty may tend to work against each other. Ultimately, the abuse that must be most carefully guarded against is that of conflicting interests, whether of prejudiced health care providers, law makers, and administrators of health insurance plans, or persons who stand to gain financially and/or relieved of responsibility by the death of a vulnerable individual.
IV. TYPES OF SAFEGUARDS
There are several ways in which safeguards against the abuse of legalized physician-assisted death can be categorized. For example, the focus could be on direct safeguards, such as wording in the new legislation specifically intended to prevent abuse, as opposed to indirect safeguards, such as increased commitment to research and development of therapeutic and palliative care treatments, so that recourse to physician-assisted death would be less likely. One of the risks of legalizing physician-assisted death could well be that the medical community and ministries of health will be less inclined to commit resources to the advancement of palliative care, since measures to short-circuit the dying process will be regarded as more cost-effective and more highly preferred by dying persons than the training of palliative care professionals and the improvement of medications and facilities designed to relieve pain, suffering and distress during the natural dying period.
The two principal classifications of safeguards against unwanted death and unwarranted interference with personal autonomy are processes before the fact (like court approval) and processes after the fact (like reporting to a state authority, and criminal prosecution for homicide). The indirect safeguards mentioned above (improvements to palliative care) are obviously "before-the-fact" safeguards. The chief problem with after-the-fact safeguards is that they only come into play once someone has died in circumstances that appear to have violated public law or policy or the rights of the deceased person. The "safeguard" is not a safeguard for that individual, who is already dead — only for other individuals by way of deterrence.
A key issue is whether safeguards can be entrusted entirely to the private context of doctor-patient-family relationships, or whether an independent agency, possibly a court, or a committee appointed by a hospital or a government ministry, should also be involved. The difficulty some may see in before-the-fact safeguards administered by some form of publicly responsible tribunal is that such bodies represent an intrusion into the privacy which ordinarily accompanies personal decisions and relationships, as well as doctor-patient confidentiality. This intrusion may be a relatively small price to pay for the assurance that such safeguards can protect in advance against abuses. The deliberations of such decision making bodies do not have to be "public" in the sense of being accessible to anyone not directly involved.
Distinctions can also be made between procedural safeguards and criteria by which to determine whether a particular case is one where physician-assisted death is an appropriate consideration (or perhaps was appropriate where after-the-fact processes come into play). Are there to be actual standards which must be met in all cases, or are the standards to be determined only in accordance with the values and wishes of individual patients? Can such different approaches to standard setting be combined?
A distinction must also be drawn between safeguards designed to protect the interests of those who are deemed to be capable of making life-or-death decisions for themselves and those who are deemed to be incapable with respect to such decisions. Attention will be paid to the issues of prior wishes competently expressed, and the elusive principles of "best interests" of a person whose personal consent (or refusal of consent) cannot be validly obtained.
It seems intuitively obvious that the most effective system of safeguards must include both before- and after-the-fact components. In other words, if the before-the-fact safeguards should ever fail to prevent what they are meant to prevent, recourse must be available after the fact to professional misconduct or criminal law sanctions as means of ensuring that in the future the before-the-fact safeguards are taken seriously.
The potential safeguards of each type (before-the-fact and after-the-fact) will be sketched out very loosely at this point, only as a preliminary way of indicating what the study will be looking for in existing or proposed laws, policies and practices, and ultimately what it will endorse as valid and useful options for consideration in Canada in the event that physician-assisted death becomes legalized.
Before-the-fact direct safeguards against unwanted death and unwarranted interference with personal choice could be described as "due process" protections. They operate on the presumption that certain procedures must be followed and certain criteria met before assisted death can happen, and on the further presumption that any health care professional involved would have known or should have known what the proper procedures and criteria are. Depending on the circumstances of each case, there may be more or less time available for the procedures to be followed. For example, if someone is expected to die within forty-eight hours, it would not make sense to follow a process that ordinarily takes two weeks to complete, unless those procedures can, depending on circumstances, be compressed into the time that is available.
The components of a before-the-fact safeguards process might include some or all of the following:
- Advance care planning on the part of individuals and families, either before the onset of a life-threatening illness or at the early stages.
- At more advanced stages of illness, obtaining second opinions, especially from professionals particularly qualified to prescribe treatments (both curative and palliative) and predict outcomes for the condition the person has.
- Family conferences at which the best available information is disclosed, the individual's best interests and wishes are discussed (including last known wishes if the person is incapable of participating in the discussion), and any professional or facility guidelines are considered.
- Referral of the situation to a hospital review committee or ethics committee which has the responsibility for ensuring that appropriate protocols are developed, disseminated and followed.
- Appointment of an independent advocate to act on behalf of the person, making sure that the individual is as fully informed as possible about various options and their likely consequences, that he or she understands what his or her rights are, both to receive medical treatment and to decide what treatment he or she wants to receive, and also that the person's wishes and decisions are being expressed without coercion or undue influence by other persons.
- Referral of the case to a court or other specialized tribunal, especially where the request is for active measures to be taken to shorten the person's life, or where a substitute decision maker is asking that life-sustaining treatment be withheld or withdrawn, and does not have an advance directive to do so from the individual. Where the individual has the capacity personally to refuse treatment that is required to sustain life, or has given clear prior instructions to that effect, such a hearing may not be necessary.
These components of a before-the-fact safeguards system are not intended to be exhaustive, and will be revisited and expanded upon towards the end of this paper. Likewise, the after-the-fact safeguards, both existing and proposed will be identified and assessed in the material which follows. The threat of prosecution or a finding of professional malpractice are obviously strong disincentives for doctors who may be asked or tempted to assist a patient to die sooner than the ordinary course of his or her illness would take. As we shall observe, however, such threats frequently fail to deter doctors from taking such action.
V. SAFEGUARDS IN CURRENT CANADIAN LAW
A. Criminal code provisions
It has already been pointed out that any positive act that intentionally causes a person's death, regardless of whether that act is intended to end the life of a person who is already clearly dying, is a violation of the Criminal Code of Canada's prohibition of homicide. It has also been pointed out that assisting a person to commit suicide, regardless of the circumstances, is a crime in Canada,29 as is administering "poison or any other destructive or noxious thing".30 Section 226 of the Criminal Code states,
Where a person causes to a human being a bodily injury that results in death, he causes the death of that human being notwithstanding that the effect of the bodily injury is only to accelerate his death from a disease or disorder arising from some other cause.
Presuming that a lethal injection is a form of "bodily injury", this section, too, seems clearly to prohibit euthanasia.
Under the Criminal Code it is also an offence to fail to provide the "necessaries of life" to anyone with respect to whom one has a legal duty to make such provision B one's child, spouse, or other person who is dependent because of disability or other cause on the individual who has the legal duty.31 This paper will consider these prohibitions below in the light of some of the actual cases that have come before the courts in recent years.
The fact that an act may be prohibited by the Criminal Code does not necessarily mean that a particular perpetrator of that act will face criminal prosecution, or that such prosecution will be successful. Given that some violations of the laws against causing death do not result in penalties for those who commit those violations means that there is a measure of uncertainty, particularly among doctors, as to whether they can escape criminal liability for assisting their patients in dying. Steps that reduce this uncertainty ought to be welcomed by health practitioners in the interests of their own personal security, and it is arguable that (depending on the nature of any legislative or administrative reforms) they will also enhance the safety and security of their patients. People ought to be able to know with as much certainty as possible what can and cannot be done in accordance with the rule of law. An examination of the criminal cases in this area (see below) reveals a great deal of hesitation, confusion and inconsistency on the part of Crown prosecutors and the courts. Persons with disabilities are placed at very serious risk by the vagaries of the current system.
According to Hugh Scher of the Council of Canadians with Disabilities,
The purpose of our criminal law is to provide protection for society, including protection from murder. The purpose of our criminal law and our criminal sentencing process is to ensure stability, certainty, public safety, and equal treatment and benefit of law to all Canadians.32
Some argue that greater consistency in applying the criminal law would follow if the Criminal Code were to be amended to provide discretionary (i.e. more lenient) sentences for so-called "compassionate homicide". This argument is based on the assumption that prosecutors, judges and juries are reluctant to subject offenders whose motivation appears to be mercy to the prospect of spending many years behind bars under the mandatory life sentence provisions of the Criminal Code as it now stands.
Hugh Scher pointed out to the Subcommittee of the Standing Senate Committee on Social Affairs, Science and Technology mandated to update "Of Life and Death" that the Criminal Code of Canada was amended in 1998 to provide extra protection for persons with disabilities against sexual exploitation33:
... People with disabilities are disproportionately victimized in these kinds of crimes. We acknowledge that disability is an aggravating factor that must be considered when we look at charging and sentencing one who is convicted of this kind of crime. When we talk about murder, why do we not also look at disability as an aggravating factor? We are in this discussion looking at disability as a mitigating factor to justify the actions of a murderer and I am concerned that that is the effect, intended or otherwise, of creating a third category of murder, the murder of vulnerable people.... To set up a completely separate category of murder which in essence amounts to a de facto acceptance of euthanasia in some respects and the denial of the equal benefit and protection of law to a particular group of people in other respects.34
If the law itself specifically jettisons existing safeguards for persons with disabilities, what hope is there of fashioning new safeguards to take their place?
B. Health care and consent laws
Health law is a matter for provincial and territorial jurisdiction in Canada. While some matters of medical malpractice may not come within the scope of the criminal law, often there are also relevant legal provisions to be found in provincial health care legislation or in civil case law. One of the common and central features of all such law is that interventions in the lives of patients by health care practitioners must ordinarily have the informed consent of the patients or of their legally authorized substitute decision makers. The ability of patients to control the actions of their care-givers through the power of giving or withholding consent to treatment is an important safeguard against abuse.
Ontario's Health Care Consent Act35 can be used as an example of a provincial statute which governs the actions of physicians and other health care professionals, including actions that may be intended to preserve or terminate the life of a patient. Some of the provisions of the Health Care Consent Act that may be relevant to the issue of safeguards in the event that the Criminal Code is amended to legalize physician-assisted death will be reviewed here.
The first safeguard, as the name of the Act implies, is that a health practitioner is not to administer any treatment unless the person "is capable with respect to the treatment, and the person has given consent; or (if the person) is incapable with respect to the treatment,... the person's substitute decision maker has given consent on the person's behalf".36 The Act goes on to state the "elements required for consent to treatment":
- The consent must relate to the treatment.
- The consent must be informed.
- The consent must be given voluntarily.
- The consent must not be obtained through misrepresentation or fraud.37
To be "informed" means that the patient (or the substitute decision maker) is told "the nature of the treatment, the expected benefits of the treatment, the material risks of the treatment, the material side effects of the treatment, alternative courses of action, (and) the likely consequences of not having the treatment".38 Section 14 of the Act states that a consent that has been given may also be withdrawn. Informed consent can only be given by someone who is "capable" of giving it. The Act defines capacity in these words:
A person is capable with respect to a treatment... if the person is able to understand the information that is relevant to making a decision about the treatment... and able to appreciate the reasonably foreseeable consequences of a decision or lack of decision.39
Being in control of the treatment one receives is an obvious safeguard against receiving unwanted treatment, especially unwanted treatment that is likely to result in one's death.
For persons who are incapable of consenting or refusing to consent to a treatment, however, the safeguard represented by the law requiring consent to treatment immediately becomes less reliable than it is for persons who are capable. The Health Care Consent Act acknowledges that fact in two ways. First, it requires substitute decision makers to abide by the wishes the person expressed while he or she was capable of making the decision in question. This represents an important safeguard against the loss of personal autonomy. If no such wish has been expressed, or if the substitute decision maker is not aware of any, then the decision is to be made that is most consistent with the incapable person's best interests.40
The notion of "best interests" sounds attractive, but it is very difficult to define in any given set of circumstances. Ordinarily, we all believe that we can determine what is in our own best interests, but how can anyone else make such a determination? Ontario's Health Care Consent Act offers some specific guidance to help substitute decision makers in medical consent matters understand what it means to act in another person's best interests. Firstly, it is necessary to put one'self in the position of the incapable person to the fullest extent possible. This means that a substitute decision maker must "take into consideration the values and beliefs that the incapable person held when capable" and "any wishes expressed by the incapable person with respect to the treatment" while the person was not capable with respect the treatment decision.41
Beyond those instructions that pertain to the wishes, values and beliefs of the individual on whose behalf a substitute decision is to be made, the Health Care Consent Act offers a fairly detailed test of what constitutes the person's best interests. The substitute decision maker is to consider the following factors:
- Whether the treatment is likely to,
- improve the incapable person's condition or well-being,
- prevent the incapable person's condition or well-being from deteriorating, or
- reduce the extent to which, or the rate at which, the incapable person's condition or well-being is likely to deteriorate.
- Whether the incapable person's condition or well-being is likely to improve, remain the same or deteriorate without the treatment.
- Whether the benefit the incapable person is expected to obtain from the treatment outweighs the risk of harm to him or her.
- Whether a less restrictive or less intrusive treatment would be as beneficial as the treatment that is proposed.42
The key components of the foregoing best-interests test are the concepts of "improvement" vs. "deterioration" of the patient's condition, and the corresponding concepts of "benefit" and "harm". The statute prefers improvement of the patient's condition over deterioration. As such, it represents a type of safeguard against physician-assisted death that is of great importance for persons who have lost or never had the capacity to make valid health care decisions for themselves.
There may be some room within these guidelines for a substitute decision to be made that would authorize measures to shorten the individual's life, if we interpret the word "well-being" to include sparing the individual from pain and suffering. Presumably the guidelines do authorize a substitute decision maker to refuse to consent to treatment that could marginally extend the individual's life span, but only in cases where the treatment is essentially futile as a means of restoring health. It must be pointed out, however, that the guidelines for determining the best interests of a patient who is incapable with respect to a proposed treatment are only matters that the substitute decision maker must consider. They are not binding.
A further potential safeguard in the Ontario legislation against abuse in making decisions about end-of-life treatment for persons who lack the personal mental capacity to make such decisions for themselves is a statutory tribunal known as the Consent and Capacity Board.43 This Board has the authority to hear and decide challenges to a health practitioner's finding that a patient is incapable with respect to a particular treatment.44 It is also empowered to appoint "a representative to give or refuse consent" on behalf of an individual who is incapable of giving consent,45 to give directions as to the interpretation of the previously expressed wishes of the individual,46 or to depart from those wishes in situations where the Board "is satisfied that the incapable person, if capable, would probably give consent because the likely result of the treatment is significantly better than would have been anticipated in comparable circumstances at the time the wish was expressed".47 Finally, the Board has the authority to determine whether a substitute decision maker is complying with the rules in s. 21 of the Act about following capable wishes or acting in the best interests of the individual.48
Some or all of the powers of the Consent and Capacity Board under Ontario's Health Care Consent Act could come into play in cases where a decision is to be made that could result in an incapable patient receiving some form of physician assistance in dying. The Board obviously has that power now with respect to decisions to withhold or withdraw life-sustaining treatment. Its powers have been outlined here because it represents another potential safeguard against abuse, not only of current provincial health care laws pertaining to substitute decision making, but also of any new federal laws that may permit physician-assisted death.
It is not suggested that the provincially appointed Board, as it is now constituted, would have jurisdiction to deal with substitute life-and-death decisions that may in the future become permissible under the criminal law, but that a similar tribunal could be introduced for the latter purpose. Conceivably the same boards, in at least some provinces, could be given both a provincial and a federal mandate, as is the case now with respect to mental health aspects of both care (eg. involuntary commitment to psychiatric facilities) and crime (i.e. disposition with respect to persons found unfit to stand trial or not guilty by reason of mental disorder). Again, it must be stressed that an individual who is incapable of personally consenting to be assisted in dying would be especially vulnerable to abuse, and therefore requires the surest possible due process safeguards against such abuse.
Of course, one does not have to be legally "incapable" in order to be victimized in the context of physician-assisted death. There are strong arguments in favour of involving the courts or quasi-judicial boards in a decision to bring an early end to anyone's life.
C. Constitutional law
The Canadian Charter of Rights and Freedoms contains two sections that are of particular relevance to the issues of physician-assisted death. These sections are s. 7, which states,
"Everyone has the right to life, liberty and security of the person and the right not to be deprived thereof except in accordance with the principles of fundamental justice", and s. 15(1):
Every individual is equal before and under the law and has the right to the equal protection and equal benefit of the law without discrimination and, in particular, without discrimination based on race, national or ethnic origin, colour, religion, sex, age or mental or physical disability.
One further provision in the Charter of Rights that must be considered is the s. 1 proviso that all of the rights it purports to guarantee are "subject only to such reasonable limits prescribed by law as can be demonstrably justified in a free and democratic society". The constitutional guarantees set out in ss. 7 and 15(1) and the limitation on Charter rights permitted under s. 1 will be examined below in the context of the relevant case law, especially in the discussion of the Supreme Court of Canada decision in Rodriguez v. British Columbia (Attorney General).49 First, they are examined on their face value.
Section 7's guarantees of life and security of the person should serve to protect persons with disabilities from any legislation or government action that would place their lives in jeopardy, unless such legislation also provided for a process that incorporates the "principles of fundamental justice". In general, such principles require that any action, authorized or undertaken by government or an agent of government, affecting an individual's life, liberty or security interests to which the individual objects, or might reasonably be expected to object, cannot be embarked upon unless a fair and impartial decision is made to do so. It is clearly arguable that any permission for substitute decision makers to choose physician-assisted death on behalf of persons who are judged incapable of making that choice for themselves would have to be accompanied by such a process. It must be pointed out, however, that no such process is required now in cases where a substitute decision is made to discontinue life-sustaining treatment or not to initiate such treatment, unless someone is prepared to challenge the decision.
Section 7 also contains the guarantee of liberty, which would tend to support those who say that the ability to choose the time and means of one's own death is an important and protected liberty. Combined with the guarantees of life and security of the person, and the due process implied in the term "the principles of fundamental justice", s. 7 of the Charter would be an underlying safeguard against the unwanted death of those who are mentally incapable of speaking their own minds on the issue, and a safeguard against the loss of personal autonomy on the part of those who are capable of making such a decision.
The equality guarantees in s. 15(1) of the Charter are designed to ensure that all Canadians are on the same legal footing when it comes to the power of governments or the legislatures to act in a manner that affects their interests. These guarantees are expressed in the most comprehensive manner possible: "Every individual is equal before and under the law and has the right to the equal protection and equal benefit of the law ..." (emphasis added). Whatever this four-fold promise means, the courts have emphasized that it is intended to correct the inequalities that have historically been inflicted on women and many minority groups. With respect to persons with disabilities, the Supreme Court's most eloquent statement of the meaning of s. 15(1) is found in the Eldridge case, in which the Court ruled that deaf persons are entitled to the assistance of sign language interpreters when they are attempting to communicate with health care providers. Writing for the Court, Mr. Justice La Forest summarized the inequalities experienced by persons with disabilities in the following words:
It is an unfortunate truth that the history of disabled persons in Canada is largely one of exclusion and marginalization. Persons with disabilities have too often been excluded from the labour force, denied access to opportunities for social interaction and advancement, subjected to invidious stereotyping and relegated to institutions. This historical disadvantage has to a great extent been shaped and perpetuated by the notion that disability is an abnormality or flaw. As a result, disabled persons have not generally been afforded the "equal concern, respect and consideration" that s. 15(1) of the Charter demands. Instead, they have been subjected to paternalistic attitudes of pity and charity, and their entrance into the social mainstream has been conditional upon their emulation of able-bodied norms.50
This paragraph captures the reality of life for persons with disabilities. It also enumerates the factors that make persons with disabilities especially vulnerable to any potential relaxation of the barriers to physician-assisted death: "exclusion", "marginalization", "stereotyping", "institutionalization", "paternalism" and "pity".
A more recent Supreme Court s. 15(1) decision, Law v. Canada (Minister of Employment and Immigration),51 though not involving persons with disabilities, devotes a great deal of attention to the general meaning of equality rights. Interestingly, the focus of the Law judgment is on the centrality of the notions of "dignity and freedom" to the Court's understanding of equality. The word "dignity" is used no fewer than seventy-nine times in the judgment. There is probably no good reason to expect that this terminology will ever be connected to the notion of "death with dignity", which is a characteristic rallying cry of those who favour legalizing various forms of physician-assisted death. On the other hand, the dignity of persons with disabilities can reasonably be associated with having a larger measure of personal autonomy. Dignity surely means that, even in cases where the individual is legally incapable of making a particular decision, his or her wishes, whether express or implied, are still regarded as the primary consideration of the person or persons who are called upon to act as the surrogate for the individual in making the decision.
In a further disability equality rights decision handed down in May, 2000, Granovsky v. Minister of Employment and Immigration52, Mr. Justice Binnie, writing for the Supreme Court of Canada, said that a discriminatory act, contrary to s. 15(1) of the Canadian Charter of Rights and Freedoms, is one that "demeans persons with... disabilities, or casts... doubt on their worthiness as human beings".53 These words would seem to apply in a situation in which death might be imposed on a person with a disability without his or her choice. They may also be relevant to the situation where a disabled person's choice of death might be disregarded, whereas that of a person without a disability would be respected. In either case, they indicate that Charter equality rights can be regarded as fundamental safeguards. It must, however, be kept in mind that the Charter is only binding on governments and those who act as agents of government.
The Supreme Court of Canada, as we have seen above in the Rodriguez case54, and will consider more fully below, has ruled by the narrowest of margins that there is no constitutional right to physician-assisted death in Canada. This does not mean, of course, that any federal or provincial statutes that may in the future authorize such assistance in dying would necessarily be ruled unconstitutional. Hopefully, however, the protections found in the Charter of Rights, especially the rights to life, security of the person and equality, will always be foundational safeguards against involuntary infliction of physician-assisted death on persons with disabilities. The guarantee of liberty in s. 7 of the Charter may also serve as a safeguard of the right to choose to be assisted in dying, if such assistance were to become lawful.
D. Case law
Whether we are considering the impact of the Criminal Code, provincial or territorial health law statutes, or the Charter of Rights and Freedoms, the ultimate test of how effective the law is in providing safeguards against abuse in relation to physician-assisted dying, is the interpretation of these various legislative provisions by the courts. The superior courts of each province and territory, the provincial and territorial appeal courts and the Supreme Court of Canada also have inherent jurisdiction, apart from their interpretation and application of statute law, to determine people's entitlements in the area of health care. The following analysis of several of the most important Canadian judicial decisions reveals that some apparent safeguards in the legislation and the Constitution are not as water-tight as they seem. On the other hand, the courts have also proposed (and in some cases imposed) their own protections against abuses.
Reference has already been made to the case of Stephen Dawson,55 in which the British Columbia Supreme Court ordered that a young boy receive needed and potentially life-saving surgical treatment despite his parents' wish that he not receive it. The judgment in the Dawson case includes several strong statements that could be drawn upon in other cases where those who have the legal authority to make substitute decisions say that they want the incapable person to die:
I am satisfied that the laws of our society are structured to preserve, protect and maintain human life and that in the exercise of its inherent jurisdiction this court could not sanction the termination of a life except for the most coercive of reasons. The presumption must be in favour of life.
I do not think that it lies within the prerogative of any parent or of this court to look down upon a disadvantaged person and judge the quality of that person's life to be so low as not to be deserving of continuance.
It is not appropriate for an external decision maker to apply his standards of what constitutes a liveable life and exercise the right to impose death if that standard is not met in his estimation. The decision can only be made in the context of the disabled person viewing the worthwhileness or otherwise of his life in its own context as a disabled person and in that context he would not compare his life with that of a person enjoying normal advantages. He would know nothing of a normal person's life, having never experienced it.56
These brief paragraphs enunciate some important rules pertaining to third party decisions in favour of death:
- The courts do not have the authority to sanction the choice of death for another person "except for the most coercive of reasons". Justice MacKenzie did not speculate what those reasons might be.
- The courts' starting-point is "a presumption in favour of life".
- "Quality-of-life" assessments of a person with a disability are not to be relied upon in making a decision that the person's life is "not deserving of continuance".
- "It is not appropriate for an external decision maker to apply his standards of what constitutes a liveable life".
MacKenzie J. thus ruled out both objective and subjective approaches that are typically used to determine that another person's life is of negative value to that person. Only the individual's personal appreciation of the value of his or her own life must determine what available measures are to be taken to preserve that life. The Dawson decision is a powerful precedent that can be referenced as a safeguard in cases where a decision in favour of death is being considered for a vulnerable person whose power of self-determination is also in question.
The decisive difference between Justice MacKenzie's approach and that of the Provincial Court Judge who first heard the Dawson case was Mackenzie J's ability to put to one side his own reflections on what it must be like to have a significant disability, and to rely exclusively on how he believed the individual feels about his or her own life. Judicial independence and impartiality must include the commitment to make decisions that are as free as possible from the force of one's own biases, as well as those of others who attempt to influence the decision-making process. Madam Justice Bertha Wilson expressed this idea in terms of a judge "entering into the skin of the litigant and making his or her experience part of your experience and only when you have done that, to judge."57
Where an individual is capable of making a health care decision and chooses to forego treatment without which he or she will likely die, the law is also now very clear. In the 1992 case of Nancy B. v. Hôtel-Dieu de Québec,58 the Quebec Superior Court ruled that a mentally capable person's wish to be taken off life supports, which had the potential to prolong her life indefinitely, must be respected. Nancy B. had Guillain-Barré syndrome, an incurable neurological disorder that left her incapable of movement. She could breathe only with the assistance of a respirator. The case stands for the proposition that a patient has a legal right to have medical treatment discontinued if he or she decides that continuation of the treatment (and of his or her life) is unacceptable.
A comparable Ontario decision is that in the case of Malette v. Shulman.59 This was a civil action by a Jehovah's Witness whose attending physician administered blood transfusions to her in spite of clear indications that she rejected such treatment on religious grounds. The Ontario Court of Appeal denied the doctor's appeal for the following reasons:
The plaintiff had a right to control her own body. The tort of battery protects the interest in bodily security from unwanted physical interference. Any non-consensual touching which is harmful or offensive to a person's reasonable sense of dignity is actionable.
A competent adult is generally entitled to reject a specific treatment or all treatment or to select an alternate form of treatment even if the decision may entail risks as serious as death and may appear mistaken in the eyes of the medical profession or of the community. Regardless of the doctor's opinion it is the patient who has the final say on whether to undergo the treatment.60
The Nancy B. and Malette v. Shulman cases have clarified the safeguards in the law against interference with a patient's right of self-determination in making a competent decision not to receive treatment that would or could prolong his or her life. The question that remains is whether this form of safeguard actually diminishes any other existing or potential safeguards against physician-assisted death in the case of those whose personal autonomy is less respected. At least one commentator has expressed the opinion that such judicial decisions have "narrowed the gap between allowing a patient to suffer natural death and medically assisting death".61
"Medically assisting death" continues to be treated as homicide by the Criminal Code of Canada. Unfortunately, the application of the criminal law by the courts is by no means as clear as is the case where non-criminal statutes and common law are concerned. There have been a number of criminal prosecutions of doctors in this country for taking active steps to accelerate their patients' deaths. None have paid a penalty commensurate with the Criminal Code's requirements for first or second degree murder. Three recent cases will be reviewed here briefly.
The first is the Ontario case of Dr. Claudio de la Rocha. His patient had lung cancer, and had been placed on a respirator. She informed family members, and they informed the doctor, that she wanted the breathing tube removed so that her suffering would end. The doctor removed the tube and administered a total of 40 mg of morphine in three doses to ensure that she did not experience a feeling of suffocation. He then administered potassium chloride, causing her heart to stop.62 Dr. de la Rocha was charged with second degree murder and with administering a noxious substance. He pleaded guilty to the second charge, and the murder charge was dropped. There was an agreed statement of facts which stated that the patient's breathing appeared to have stopped before Dr. de la Rocha administered the potassium chloride. He was given a three-year suspended sentence.63 He was also disciplined by the Ontario College of Physicians and Surgeons and given a 90-day suspension from the practice of medicine.64
Mr. Justice Loukidelis stressed that the leniency of Dr. de la Rocha's sentence was not to be taken as an indication of approval of physician-assisted death. He wrote:
If a medical doctor administers a lethal dosage of a drug or substance in order to kill a patient for the purposes of euthanasia, in my view that is a breach of the law and is deserving of severe punishment C not only severe punishment by sanctions (as suggested by the Crown) but should be attended with a long period of imprisonment.... He also has to know that the principles of life are not excepted for people who face overwhelming disease and are at the point of death's door.65
The "principles of life" lie at the heart of the criminal law's persistent prohibition of acts which cause death. Those principles need to be articulated as safeguards for vulnerable persons, even if at some future point the law should relax those prohibitions. As we have seen, some of those principles have already been identified by Justice MacKenzie in the Dawson decision in the Supreme Court of British Columbia.66
Another case which has attracted a great deal of media attention is that of Dr. Nancy Morrison in Halifax. Late in 1996 she had a patient who was also in the terminal stages of cancer, and his family asked that he be taken off life supports. Dr. Morrison complied. As in Dr. de la Rocha's case, she administered morphine, followed some time later by potassium chloride, with the obvious intention of ending the patient's life. She was initially charged with first degree murder, but the charge was later reduced to manslaughter. Eventually the charges against Dr. Morrison were dismissed. The fact that the patient had not been helped by large doses of morphine and other drugs gave rise to conjecture that the intravenous tubing was blocked, and that the lethal drug she administered to the patient did not actually cause his death. Dr. Morrison admitted having administered a lethal injection of potassium chloride in professional misconduct proceedings conducted by the Nova Scotia College of Physicians and Surgeons, which issued a reprimand.67
The final case in this brief trilogy of criminal prosecutions of doctors who assisted their patients to die is R. v. Genereux.68 Dr. Genereux pleaded guilty to aiding and abetting suicide after prescribing lethal doses of Seconal to two men who were HIV-positive, but who did not have AIDS symptoms. The doctor had no way of knowing that either of the two men was terminally ill. He did know that treatment could have helped them both. Both men acquired and consumed the drugs. One died, but the other was revived after a friend called 911.69 Dr. Genereux was sentenced to a term of imprisonment of two years less a day, to be followed by three years' probation. The Court of Appeal upheld the sentence, stating that:
... the trial judge was alive to the seriousness of the appellant's crimes and to the values sought to be protected by s. 241(b) of the Criminal Code,... the preservation of life and the protection of vulnerable people. (These patients) were the kind of people s. 241(b) should protect. Each was sick, confused, frightened and intent on suicide. But each could have been treated, as neither was terminally ill.70
The appeal judges were also concerned about the impact a lengthy prison term in Dr. Genereux's case would have on other physicians. They wrote, "We doubt the wisdom of imposing a sentence designed to, or that might, intimidate physicians in the appropriate treatment of their patients".71 In other words, a "get tough" policy may be counterproductive, because it would discourage doctors from offering appropriate medication to relieve pain and suffering, and from terminating life-sustaining treatment when it becomes futile and is no longer wanted by their patients. This principle must be taken into account when evaluating safeguards for persons with disabilities. Making one person safe from death may make others vulnerable to being undertreated or overtreated in order to prolong life, and to avoid criminal liability at all costs.
Before his case was concluded in the courts, Dr. Genereux had been deprived of his licence to practise medicine by the College of Physicians and Surgeons of Ontario.
It is interesting to note that, of the three physicians whose criminal cases have been mentioned here, the only one who actually went to prison, and who lost permanently his right to practise medicine was Dr. Genereux, who was charged not with murder, but with aiding and abetting suicide. It would appear that the criminal justice system, given that the current laws are in place, is more lenient towards those who actually kill dying patients than it is towards those who assist non-dying patients to take their own lives. However, the distinguishing factor in his case is no doubt the fact that his patients were not at the point of death, and indeed neither was terminally ill. Be that as it may, the threat of criminal prosecution, while serious, leaves physicians confused and uncertain.
The real landmark case in Canada on the issue of physician-assisted death is Rodriguez v. British Columbia (Attorney General).72 Sue Rodriguez had amyiotrophic lateral sclerosis. She faced the prospect of not being able to survive without extensive life supports. Her wish was that, when she reached the point at which she believed her life was no longer tolerable, she could end it with the assistance of a physician. Her case was a challenge to the constitutionality of s. 241(b) of the Criminal Code, which prohibits aiding or abetting a person to commit suicide. The challenge was based on sections 7, 12 and 15(1) of the Canadian Charter of Rights and Freedoms. None of the Supreme Court justices regarded the prohibition of assisted suicide to be "cruel and unusual treatment" in the language of s. 12.
The five-member majority of the Court rejected all of the constitutional claims. Section 7 states that "Everyone has the right to life, liberty and security of the person and the right not to be deprived thereof except in accordance with the principles of fundamental justice". The majority agreed that "Fundamental justice requires that a fair balance be struck between the interests of the state and those of the individual".73 Section 241(b) of the Criminal Code was described as in keeping with the government's objective of "protecting the vulnerable". The majority were of the view that, "Given the concerns about abuse and the great difficulty in creating appropriate safeguards, the blanket prohibition on assisted suicide is not arbitrary or unfair".74
The majority in Rodriguez agreed with the minority opinion of the Chief Justice and Justice Cory that s. 241(b) of the Criminal Code does in fact violate s. 15(1) of the Charter by discriminating against those whose disabilities are so severe that they are unable to commit suicide without the assistance of another. However, unlike the Chief Justice and Cory, J., the majority simply assumed without deciding that Ms. Rodriguez's equality rights were violated by s. 241(b). They had no difficulty in excusing the violation as a reasonable limit on the right to equality, which is permitted by s. 1 of the Charter. The purpose of s. 241(b) "is to protect and maintain respect for human life" and "to protect life and those who are vulnerable in society". The blanket prohibition of assisted suicide was found to be "reasonably justified" because it is "the best approach" to the achievement of those goals.75 The reasoning of the majority is summarized in the headnote of the decision,
In order to protect life and those who are vulnerable in society effectively, a prohibition without exception on the giving of assistance to commit suicide is the best approach. Attempts to modify this approach by creating exceptions or formulating safeguards to prevent excesses have been unsatisfactory.76
David Lepofsky has taken issue with the majority in Rodriguez for presuming to decide that a violation of a Charter equality right is excusable under s. 1 without analysing the severity of the s. 15(1) infringement of the individual's equality rights. In effect, Lepofsky asks, how can issues of justification be decided without looking at the seriousness of the deprivation of equality? He presumes that the denial of an extremely important equality right requires a correspondingly "weighty section 1 justification".77 He also castigated the majority for focussing on the general societal impact of invalidating the law prohibiting assisted suicide, rather than on the specific impact of allowing a constitutional exemption in Sue Rodriguez's case. However, even the Chief Justice's dissenting opinion points out that a constitutional exemption is only available as an interim measure when the impugned law is declared invalid, but the invalidity is suspended to allow Parliament to consider what the appropriate legislative remedy might be.78
Finally, Lepofsky questioned the majority's conclusion that "... it was impossible to devise a system of safeguards sufficiently rigourous to ensure that a vulnerable person is not assisted to die over his or her objection". Lepofsky contended,
Surely it would be possible to invent a system which would allow for assisted suicide only (when) sufficient demanding, multi-faceted safeguards are deployed, such as court approval, substantial time delays or 'cooling off' periods after the person requests assistance, independent investigation to detect possible undue family pressure, and the like.79
We will consider shortly these various potential safeguards as they were proposed and evaluated in Chief Justice Lamer's dissenting judgment.
Justices L'Hereux-Dubé and McLachlin dissented from the majority judgment in Rodriguez solely on the grounds that s. 241(b) of the Criminal Code infringes the right to security of the person included in s. 7 of the Charter. They defined this right to include "personal autonomy, which protects the dignity and privacy of individuals with respect to decisions concerning their own body". These two justices would have wanted "a stipulation requiring a court order to permit the assistance of suicide in a particular case only when the judge is satisfied that the consent is freely given", in order to "ensure that only those who truly desire to bring their lives to an end obtain assistance".80
The Chief Justice wrote more extensively on the safeguards that he thought should be in place if, as he would have ruled, the Criminal Code prohibition of assisted suicide should be struck down and, in the interim, a constitutional exemption were to be ordered permitting Sue Rodriguez to commit suicide with the assistance of a physician. He listed those safeguards as follows:
- An application must be made to a superior court for permission to terminate one's life.
- The applicant must be certified by a treating physician and independent psychiatrist to be competent to make the decision to end her own life, and the physicians must certify that the applicant's decision has been made freely and voluntarily.
- At least one of the physicians must be present with the applicant at the time the applicant commits assisted suicide.
- The physicians must also certify that the applicant is or will become physically incapable of committing suicide unassisted, and that they have informed the applicant that he or she has a continuing right to change his or her mind about the decision to terminate life.
- The Regional Coroner must be given notice and an opportunity to be present at the examination of the independent psychiatrist.
- The applicant must be examined daily by one of the certifying physicians to ensure that he or she still wants to take his or her own life.
- The constitutional exemption will expire if the dying person has not exercised the option within 31 days from the date of examination by the independent psychiatrist.
- The act causing the death of the applicant must be that of the applicant him or herself, and not of anyone else.81
These safeguards will be discussed below in the context of the discussion of the work of the Special Senate Committee on Euthanasia and Assisted Suicide, where they received considerable attention. Before leaving them, however, it is worth pointing out how heavily medicalized they are. Catherine Frazee has asked, "Just as disability scholars have challenged the medical model of disability, is there not a similar critical analysis to be made of death as a medical construct? Surely there are alternative ways (social, cultural, spiritual and even political ways) of conceptualizing and interpreting death?"82 This warning against a narrow, physician-focussed approach to the issues of life and death must be kept in mind whenever we encounter and evaluate the various notions about assistance in dying and the construction of safeguards to ensure equal protection for vulnerable persons.
VI. PROCESSES AND PROPOSALS TO REVIEW AND CHANGE CANADIAN LAW
A. Senate Committee on Euthanasia and Assisted Suicide
A Special Committee of the Senate of Canada, appointed on February 23, l994, undertook "to examine and report on the legal, social and ethical issues relating to euthanasia and assisted suicide".83 After hearing testimony from individuals and groups all across Canada, the Committee issued its final report, "Of Life and Death" in June, 1995. The report includes findings and recommendations with respect to palliative care, pain control and sedation processes, withholding and withdrawal of life-sustaining treatment, advance directives, assisted suicide, euthanasia and compassionate homicide.
The Committee made several recommendations, some pertaining to policy and others to proposed changes in the law. Many of the recommendations were unanimous, but the members were unable to achieve consensus on some significant issues. In some of its recommendations and in the testimony of witnesses who appeared before the Committee, a number of safeguards were identified against the abuse of end-of-life health care and assistance-in-dying procedures. Many of these safeguards, which will be examined in detail below, are of particular interest to vulnerable persons.
The Committee recommended giving greater priority to palliative care and to the development of more effective means of pain control. These are major safeguards against the use, let alone abuse of physician assistance in dying. The Committee recommended that "the Criminal Code be amended to clarify the practice of providing treatment for the purpose of alleviating suffering that may shorten life", and "to explicitly recognize and to clarify the circumstances in which the withholding and withdrawal of life-sustaining treatment is legally acceptable".84
The Senate Committee recommended that there be no change to the Criminal Code provisions banning counselling, and aiding or abetting suicide, and that all forms of euthanasia remain a criminal offence. However, there were minority recommendations that an "exemption to subsection 241(b) of the Criminal Code (prohibiting assisted suicide) be added, under clearly defined safeguards, to protect individuals who assist in another person's suicide", and that "voluntary euthanasia" be either permitted or be made subject to a less severe penalty.85 The minority recommendation also included that "in order to avoid abuse, procedural safeguards must provide for review both prior to and after the act", whether of assisted suicide or voluntary euthanasia.86
The Senate Committee also recommended that "the Criminal Code be amended to provide for a less severe penalty in cases where there is an essential element of compassion or mercy". The Committee recommended that this could take the form either of "a third category of murder" or "a separate offence of compassionate homicide".87
The safeguards set out in the final report of the Senate Committee on Euthanasia and Assisted Suicide are primarily contained in the testimony of some of the witnesses who appeared before the Committee. Since the Committee itself decided against relaxing the existing prohibitions of assisted death, there was less reason for it to focus on safeguards. The favoured safeguard was to maintain the criminal sanctions currently in place. A minority of Committee members, however, would have recommended "an exemption to the Criminal Code that would permit persons to assist in a suicide under clearly defined safeguards". These members were of the opinion that the current criminal prohibitions are not working, but that they could be relaxed and at the same time made more effective. They believe that, at present, assisted suicide is taking place despite its illegality and it is occurring without adequate controls. Thus there is more potential for abuse because there is a greater risk to the vulnerable from unregulated medical assistance at the end of life, than from legislative changes accompanied by appropriate safeguards.88
At a minimum, these minority senators regarded the following as essential elements in such safeguards:
The individual must be competent and must be suffering from an irreversible illness that has reached an intolerable stage, as certified by a medical practitioner.
The individual must make a free and informed request for assistance, without coercive pressures.
The individual must have been informed of and fully understand his or her condition, prognosis and the alternative comfort care arrangements, such as palliative care, which are available.
The individual must have been informed of and must fully understand that he or she has a continuing right to change his or her mind about committing assisted suicide.
A health care professional must assess and certify that all of the above conditions have been met.
No person should be obligated to provide assistance with suicide.89
The minority Committee members were also of the view that
... regulations must be established in order to deal with the monitoring and enforcement of the safeguards by the appropriate level of government and that records must be maintained of all applications for and instances of assisted suicide. In order to avoid abuse, the safeguards must provide for review both prior to and after the act of assisted suicide.90
The Committee report does not specify what nature these reviews ought to have. No mention is made, for example, of the necessity of an application to a court, such as Chief Justice Lamer insisted upon as a primary criterion in his dissenting judgment in Rodriguez.
It must be noted that nowhere in the minimum guidelines proposed by the minority of senators on the Committee does it say that a physician is the only person who would be permitted to assist an individual in committing suicide. A "medical practitioner" would have to certify that the individual was mentally capable of making the decision to end his or her life, and that the patient's illness was irreversible and his or her suffering intolerable. A "health care professional" would be responsible for certifying that the request for assistance in dying was properly informed and free of "coercive pressures", that the person knew about "comfort care" alternatives to assisted death and that the decision to commit suicide was never final until the act itself had been performed. Possibly the avoidance of any requirement that a physician must provide the actual assistance was in deference to the number of doctors and medical organizations who had testified before the Committee that they were opposed to any scheme that would cast the members of the medical profession in the role of killers, rather than healers.
Many of the witnesses who appeared before the Senate Committee on Euthanasia and Assisted Suicide expressed strong views opposing the legalization of assisted death on grounds that no system of safeguards could adequately protect the interests of vulnerable persons, and that alternative approaches have not been adequately pursued. For example, Dr. David Roy told the Committee
It is illusory, or at least highly questionable, that a society would be able to uphold the voluntary character of euthanasia once it became legally, socially and ethically acceptable for many people. It would be difficult, if not impossible, to construct a law that would prohibit people from using persuasion, however subtle, on people to request euthanasia when that is probably not what they want.
I have seen that, particularly with respect to AIDS patients who have been totally abandoned by their parents, brothers and sisters and by their lovers. In a state of total isolation, cut off from every source of life and affection, they would see death as the only liberation open to them. In those circumstances, subtle pressure could bring people to request immediate, rapid, painless death, when what they want is close and powerful support and love.91
It may well be possible to create an extensive regime of safeguards other than the strict prohibition of assisted death currently legislated in the Criminal Code, but is it possible to ensure for every person "close and powerful support and love"?
The Senate Committee reviewed the extensive safeguards proposed by Chief Justice McEachern of the British Columbia Court of Appeal, who dissented in the 2-1 judgment in that Court that Sue Rodriguez should not be granted an exemption from the Criminal Code prohibition of assisted suicide.92 These formed the basis for Chief Justice Lamer's requirements in his dissent in Ms. Rodriguez's subsequent appeal to the Supreme Court of Canada.
McEachern, C.J. called for an application to be made to a superior court for permission to terminate one's life. The fact that the individual is mentally competent to make such a decision and is doing so of his or her own free will would have to be verified by both a "treating physician" and a psychiatrist. One of these physicians would have to be present when the death occurred, and the psychiatrist would have to have examined the applicant not more than twenty-four hours previously. At least three days before that, notice would have to be given to the Regional Coroner, who would have the authority to be present, or to nominate another physician to be present, "at the examination of the person by a psychiatrist in order to be satisfied that the person does, indeed, have mental competence to decide and did, in fact, decide to terminate his or her life". In addition,
One of the physicians giving any certificate as aforesaid must re-examine the person each day after the above-mentioned arrangements are put in place to ensure that the person does not evidence any change in his or her intention to end life. If the suicide is carried out, such physician must furnish a further certificate to the Coroner confirming that, in his or her opinion, the person did not change his or her mind.93
Fortunately for the physician, this process need not go on for more than thirty-one days, because the original certificate would then expire.94 Chief Justice McEachern did not make a recommendation regarding any process that would have to take place after the death of the individual. The Senate Committee Report lists twelve "minimal safeguards" proposed in his submission by Russel Ogden, then a graduate student in criminology. Ogden's list of safeguards includes virtually all those mentioned by other witnesses and adds some interesting one's. For example, he proposes that
Counselling should be available for the patient and other persons involved with respect to the following: possible treatment alternatives, the diagnosis and prognosis, the consequences of the aid-in-dying procedure, the underlying motivation for requesting euthanasia, and alternative care environments.95
He also told the Committee that there should in each case be an assessment intended to detect "treatable depression".
Ogden published his policy analysis and proposals in the form of draft legislation about the same time the Senate Committee was conducting its hearings.96 His proposed legislation will be reviewed under the heading of "Other legislative proposals" below.
The Senate Committee received two sample amendment proposals from witnesses from the academic community, which were included in an Appendix to the report. These proposals, outlined by Professors Bernard Dickens and Eike-Henner Kluge, contain some procedural safeguards that are not unlike those suggested by Chief Justice McEachern of the British Columbia Court of Appeal and Chief Justice Lamer of the Supreme Court of Canada in their minority judgments in the Rodriguez case.
Professor Dickens proposed that "a person physically incapable of suicide should be able to apply to a court", which would have the authority to "give a specified person a discretion, as opposed to a duty, to act; that is, the applicant would have no 'right-to-die', and the specified person would have no 'duty to kill'".97 Accompanying this formal before-the-fact procedure, Professor Dickens advocated the establishment of a "third degree murder" category, to be distinguished from first or second degree murder on the basis of "the victim's competent request made outside a judicial approval". Without such approval or competent request, killing "would remain punishable probably as first degree murder".98 Third degree murder would not be subject to the mandatory periods of imprisonment before eligibility for parole that exist with respect to first and second degree murder. Professor Dickens suggested that the punishment for third degree murder should be at the discretion of the trial judge, who "would cater the punishment on conviction to the evidence of the circumstances".99
Professor Kluge's recommendations touched on both "palliative measures" and "voluntary euthanasia". He proposed that the Criminal Code be amended to the effect that, whenever a palliative measure "will or is likely to" shorten a patient's life by a period greater than "would normally be expected using [other] appropriate and recognized palliative measures, the case shall be subject to review by an independent body" consisting of three independent persons: a physician, a member of the Attorney General's Department, and "an independent member of the public having training in ethics". This tribunal would only have authority to determine whether the proposed palliative measure "was in accordance with the competently expressed wishes of the patient or in accordance with appropriate standards of proxy decision making". Failing that, "the otherwise relevant provisions of the Criminal Code shall apply".100 This would be an interesting combination of both before-the-fact and after-the-fact safeguards. It would provide a health care practitioner with a definitive answer as to whether the proposed measure was legally acceptable. One problem with this approach is that, once approved, the palliative measure would potentially become the standard against which other more lethal measures would be assessed, which would formalize the "slippery slope" phenomenon.
With respect to voluntary euthanasia, Professor Kluge's suggestions were again somewhat novel. The key element would be "the fundamental values of the person". Voluntary euthanasia would be permitted, upon an application to a superior court, where "a person suffers from an incurable and irremediable disease or medical condition, and... that person experiences the disease or condition as violating the fundamental values of that person". In cases where the patient lacks the mental capacity to state what his or her fundamental values are with respect to the impact of the disease or to having his or her life terminated, and has never competently expressed what they are, the court would be required to determine the applicable values "in consultation with" a five-member advisory panel consisting of
- a duly empowered representative of an association for handicapped persons;
- a practising physician;
- a practising nurse;
- a person having expertise in biomedical ethics; and
- a member of the public at large.101
It is very interesting to see at the top of the list a representative of an association for handicapped persons, especially since the author of the proposal a decade or so earlier had publicly stated that when Stephen Dawson received the surgery he needed to save his life, he had been subjected to "the injury of continued existence", given the serious nature of his disabilities.102 Aside from the difficulty a court may have in dealing with the notion of an individual's "fundamental values", and in attempting to determine such values "in consultation with" a group of people who are not identified as witnesses, acknowledgement must be made of the merit of including in that group a person who speaks on behalf of persons with disabilities. Unfortunately, there is no mention of anyone with expertise in palliative care.
B. Senate Subcommittee Update of Life and Death - June, 2000
In November, 1999, the Canadian Senate adopted a motion authorizing the Standing Senate Committee on Social Affairs, Science and Technology to "examine and report upon developments since the tabling in June 1995 of the final report of the Special Senate Committee on Euthanasia and Assisted Suicide". The Subcommittee which carried out this review tabled its report 103 on June 6, 2000, the fifth anniversary of the tabling of the original report, Of Life and Death. Its mandate was to hear witnesses and to deliberate on whatever actions had been taken in the intervening five years on the unanimous recommendations made by the original Senate Committee. The Subcommittee concluded that "overall, progress on the 1995 unanimous recommendations has been insignificant or non-existent".104
Perhaps the most telling part of the June 2000 Senate Subcommittee report is its title: Quality End-of-Life Care: The Right of Every Canadian. This is a significant departure from the focus inherent in the name given to the original Senate Committee "on Euthanasia and Assisted Suicide". The new focus on care, rather than on death, was of course dictated in part by the restriction that the update would only consider progress made on the unanimous recommendations made in 1995. The Senate Committee on Euthanasia and Assisted Suicide had failed to reach unanimity on both euthanasia and assisted suicide. As noted above, changes in the law to permit these two types of acts were only supported by a minority of the Senators on the original Committee. The Subcommittee to update Of Life and Death accordingly confined their investigations to "the progress made on implementing the unanimous recommendations made in the 1995 report... with respect to palliative care, pain control, sedation, withholding or withdrawing life-sustaining treatment, and advance directives".105
The June 2000 update by the Senate Subcommittee observed that "calls for a more compassionate and comprehensive approach to end-of-life seem to be assigned a low priority in the existing health care system". The Subcommittee's Conclusions state that "the principles, expertise, and medical infrastructure required for the care of people facing death were evolving far too slowly" and that "quality end-of-life care will not happen unless the federal government takes a leadership role in developing a national end-of-life care strategy".106
The Subcommittee heard evidence that the death rate in Canada is growing, due to an aging population and increasing incidence of often terminal illnesses such as cancer, AIDS, and cardiovascular disease. In spite of these statistics, there had been "no equivalent increase in palliative programs", and only "an estimated 5% of dying Canadians receive integrated and interdisciplinary palliative care". "Palliative care" was defined in Of Life and Death as "care aimed at alleviating suffering B physical, emotional, psychosocial, or spiritual B rather than curing".107
In Quality End-of-Life Care the Senate Subcommittee decries the lack of research, training, and strategizing in the area of palliative care, and yet states that "the trend is away from an ethic of prolonging life at all costs and toward an ethic that emphasizes the quality of life and of dying". Obviously this trend is not evident in practice, but only in theory. The report pinpoints particular areas in which practice is lagging especially far behind the emerging palliative care principles: home care, people living in isolated regions of the country, Aboriginal peoples, prison inmates with AIDS, and people with disabilities.108
The Subcommittee heard fresh evidence on the role played by advance directives in end-of-life care. Advance directives are of two types: "instruction directives" (telling physicians what treatments in what circumstances the patient does or does not wish to have) and "proxy directives" (identifying the person or persons who are authorized to make substitute medical decisions for patients who no longer are capable of doing so for themselves). Again, the Subcommittee came to believe that practice is not in step with theory:
Most of (the) problems are associated with the traditional view of advance directives as based on the principle of the patient's autonomy, and the witnesses noted that advance directives are now best seen as part of a planning and communication process that helps people prepare for death in the context of their loved ones.109
This allusion to changing principles in the areas of advance and surrogate decision making is challenging, and not sufficiently elaborated in the report to enable its validity to be properly assessed. It could be interpreted as the sacrifice of personal autonomy to the interests and biases of others, or, more positively, as the recognition of supported, consensus-based decision making as the norm which ordinarily applies in the context of family life. Very few people ever make critical decisions, including those at the end of life, in a social vacuum. But far too many people with disabilities experience their social milieu as depriving them of genuine autonomy, entitlement, personhood and worth.
How can the reality that most persons approach death surrounded by at least a few other people who have strong feelings about what is happening, be harnessed as a force for the individual's total well-being? The easily tossed-off phrase "loved ones" at the end of the above-quoted passage does not inspire confidence that the Subcommittee recalled in any serious way David Roy's insistence before the 1995 Senate Committee that "close and powerful support and love"110 is what people really want as they enter the dying process.
Catherine Frazee has pointed out that the dynamic of a patient being truly loved would naturally relate to the provision of appropriate palliative care, since the primary wish on the part of those who love the patient would be for that person's symptoms and pain, of whatever sort, to be relieved by means other than by causing his or her death.111 Only secondarily, and in the rare circumstance where no relief can be obtained in any other way, would it be consistent with the nature of love to approve of the intentional shortening of the patient's life.
The June 2000 Senate Subcommittee report has very little to say about practices which actually hasten death, other than to lament that virtually no research has been done pursuant to the recommendations in Of Life and Death on the issues of withholding or withdrawing life-sustaining treatment. They also noted that the recommended research on "total sedation" (the practice of rendering a person totally unconscious through the administration of drugs without potentially shortening life) had not been done. The Subcommittee heard evidence that "there is general agreement that rarely, if ever, will properly administered pain control shorten life".112
One research result flowed from the 1995 Senate Committee recommendation that research be undertaken to determine the numbers of persons who ask for euthanasia, their reasons for doing so, and the impact on such requests when alternatives are proposed:
Research has linked depression to a desire to hasten death and there is a particular need for evaluative research to determine the effectiveness of interventions and programs that may reduce any desire for a premature death in the terminally ill.113
Once again, the thrust of the Senate Subcommittee's thinking seems to have shifted from a euthanasia perspective to one showing concern that Canada's health care system become more attuned to support vulnerable persons and to give people with terminal illnesses cause to want to live out their days, and to do so with as little distress as possible, rather than to seek an early death.
The Subcommittee was able to report that several professional organizations, between 1995 and 2000, have "individually and collaboratively developed codes of ethics and joint statements on many key issues". Unfortunately, the report does not include these documents, although two of them are referred to in an appendix listing the materials received by the Subcommittee.114
One final item of considerable interest appears near the end of the Senate Subcommittee's June 2000 report. In a paragraph that re-iterates the original 1995 recommendations that the law pertaining to end-of-life medical decisions needs to be clarified, the report says,
However, legislation should not become an attempt to micromanage medical practice; legislation cannot substitute for good judgement, good practice and an understanding of the appropriate medical ethics.115
This returns us to the question as to whether safeguards should be legislated or found in professional codes of ethics. The obvious answer is "both", but obvious answers are not invariably correct.
C. Other legislative proposals
There have been several attempts to amend the Criminal Code prohibitions of aiding and abetting suicide by way of private members bills in Parliament. Some of these bills have also included what their authors regarded as clarifications of the law governing the withholding or withdrawal of life-sustaining treatment. There has also been at least one Canadian proposal (that of Russel Ogden) for the creation of a non-criminal alternative legislative scheme for the regulation of physician-assisted death.
The most recent private member's bill, Bill S-2, was introduced by Senator Sharon Carstairs in the Canadian Senate in October, 1999. The focus of Bill S-2 is on "the medical practices of the withholding and withdrawal of life-sustaining treatment and the provision of treatment to alleviate suffering that might result in the shortening of life".116 There is no reference in the Bill to assisted suicide, euthanasia or compassionate homicide. The Bill's subtitle, "An Act to facilitate the making of legitimate medical decisions regarding life-sustaining treatments and the controlling of pain" (emphasis added) suggests that it does not create new law. Upon examination, this is in fact largely the case.
Given the short title, the Medical Decisions Facilitation Act, the legislation would exempt "health care providers" from liability under the Criminal Code for certain acts described in the Bill. Section 2 of Bill S-2 states that
No health care provider is guilty of an offence under the Criminal Code by reason only that the health care provider, for the purpose of alleviating the physical pain of a person but not to cause death, administers medication to that person in dosages that might shorten the life of the person.
Section 3 states that
No health care provider is guilty of an offence under the Criminal Code by reason only that the health care provider withholds or withdraws life-sustaining medical treatment from a person who has made a request... that the treatment be withheld or withdrawn.
Section 3 goes on to say that
Where a person who is not competent and did not while competent make a request [that treatment be withheld or withdrawn], the request may be made... by a legal representative having the authority to make health care decisions on behalf of the person, or... by the spouse, companion or relative who is most intimately associated with the person.
All of these actions are immune to criminal prosecution as the law in Canada stands now. However, the issue of a surrogate decision maker having the authority to order that no further life-sustaining treatment be given to a person who lacks the mental capacity to make such a decision for himself or herself is one that calls for particular safeguards in keeping with the principles set out by Justice MacKenzie in the Dawson case,117 and in provincial or territorial health care decisions legislation.118 The law governing these matters is essentially the same now as it would be after the enactment of Bill S-2.
The one feature of Bill S-2 that may represent new law is the definition of "life-sustaining medical treatment" in s. 4 of the Bill to include "artificial hydration and nutrition". The Euthanasia Prevention Coalition of Ontario has expressed serious reservations about this provision:
If Bill S-2 becomes law, Section 4 of the Bill may result in the intentional starvation and dehydration of elderly, disabled or incompetent (vulnerable) patients who are not terminal.... When it becomes an acceptable practice to dehydrate and starve people to death, even if they are terminal, then it will be argued that it is more humane to kill them with a needle.119
The qualifier "artificial hydration and nutrition" calls for a definition which the Bill fails to provide. Does the fact that fluids and nutrients are administered other than by mouth make them "artificial"? The connotation, quite possibly by design, is to characterize any out-of-the-ordinary means of receiving nourishment and hydration as somehow "unnatural", and therefore as "medical" interventions that can and often should be dispensed with. Basic human functions such as eating and drinking should not be equated with measures which are only considered in response to illness or injury. Eating and drinking are everyday activities for every living person, and to the extent that it is possible they should continue to be so until death, and not be withdrawn as a means by which to cause death.
Section 6 of Bill S-2 calls for the federal Minister of Health to take the initiative "with provincial authorities and associations of health care professionals" to promote "the establishment of national guidelines for the withholding and withdrawal of life-sustaining medical treatments, for the controlling of pain, and for palliative care". This, again, is obviously not something that requires new legislation. If such "national guidelines" are to be developed, then the issue of safeguards for vulnerable persons should be recognized as a priority.
Russel Ogden's proposed "Aid-in-Dying/Euthanasia Act"120 is an attempt to construct a system that would operate as a safe detour for physicians around the existing Criminal Code prohibitions, including those which currently prohibit assisted suicide and active voluntary euthanasia. A central feature of Ogden's proposed legislation is the creation of "Aid-in-Dying Boards", appointed by the provincial or territorial minister of health, and composed of individuals drawn from "a cross-section of professional backgrounds". The "selection criteria", according to Ogden, "should be based on principles of ethics, liberalism, and civil libertarianism".121 On the other hand the "selection criteria" by which the Boards would determine whose applications for aid-in-dying would be approved are unstated. Bodies that are given quasi-judicial authority over as important a matter as life and death should presumably be given some legislated standards which they would be required to apply.
Persons who wish to have assistance in dying (or their proxies) would submit an "Application for Aid-in-Dying" to a Board with the assistance of an "Aid-in-Dying Counsellor". These counsellors would have special training, and would lead the applicants through an intensive program of learning and self-examination, as well as conducting their own assessments of the applicants' mental capacity and whether they may have treatable depression. They would make recommendations to the Aid-in-Dying Board regarding the application. The Board would issue (or refuse to issue) an Aid-in-Dying Licence, which would remain valid for up to three months. If the Board refused to issue the licence, the applicant would have the right to appeal directly to the Minister of Health. Aid-in-Dying would be "under the supervision of a qualified medical practitioner", but the actual administration of the lethal substance could be done or assisted by any adult. After the applicant has died, a report would have to be submitted both to the Aid-in-Dying Board and to the Coroner's Office.122
Ogden's draft legislation defines a "proxy" as "a surrogate appointed by a patient to make treatment decisions, including euthanasia" (emphasis added). It would appear that making applications for aid-in-dying would not be within the authority of any other legally appointed substitute decision makers or relatives of individuals who lack the required mental capacity to make a decision to hasten the end of their lives. At least, under this model, euthanasia would be restricted to those who actively ask or plan for it.
Ogden lists a number of "safeguards" which he believes his scheme includes:
voluntary participation for applicants and physicians, Aid-in-Dying Boards, counselling regarding decision-making and treatment alternatives, assessment of ability to make informed medical consent decisions, time-limited Aid-in-Dying licences, restrictions on who may request euthanasia on behalf of individuals, medical supervision of Aid-in-Dying procedures, independent third party witnessing of applications, reviews by the Minister of Health.123
One safeguard Ogden seemingly failed to contemplate was to include spokespersons for vulnerable people on his "Aid-in-Dying Boards". Appointing people from "a cross-section of professional backgrounds... based on principles of ethics, liberalism, and civil libertarianism" would arguably perpetuate a bias against persons with disabilities, unless their voice was always heard in the discussion of whether it is appropriate to accept at face value an application for aid in dying. As noted above, Professor Kluge was careful not to make the same mistake.124
VII. DEVELOPMENTS OUTSIDE CANADA
A. United States litigation
In the late 1980's there was a series of high-profile court cases in the United States initiated by persons with disabilities who wished to be assisted in dying by means of the withdrawal of life supports.125 These cases might be regarded as "passive euthanasia" cases. As we have seen in the Canadian context, there is a right to refuse treatment, even if the individual will undoubtedly die without it. The key issue in the U.S. cases was the evidence that these persons wished to die because they believed their disabilities made their lives not worth living. The courts tended to ignore the evidence that the petitioners were victims of society's failure to provide the supports they required in order to live a meaningful life. In at least one case, McAfee, even though the court approved the petition, disability activists were able to assist him to discover that he could live his life without the dependency and stigmatization that had led him to seek death. The important message that lingers after this line of cases is that there must be the same dedication on society's part to the prevention of suicide by persons with disabilities as there is when suicidal persons do not have apparent disabilities.
In 1997, two cases challenging the constitutional validity of State legislation banning physician-assisted suicide found their way to the Supreme Court of the United States.126 These cases originated in the States of Washington and New York. In both cases the respective Circuit Courts of Appeal had struck down the ban. In both, the U.S. Supreme Court was unanimous in upholding it.
The Washington case was based on the Due Process Clause of the Fourteenth Amendment to the American Constitution. The four physicians who had brought the action against the State argued that the Due Process Clause protects citizens' liberty interest in being able to control their own time and method of dying. The New York case invoked the Fourteenth Amendment's Equal Protection Clause. Again, a group of physicians argued that patients who express a competent wish to have life-sustaining treatment terminated are permitted to do so. Why, then, should not similar patients be permitted to self-administer prescribed drugs that would end their lives? The Court rejected both the liberty and equality arguments for essentially the same reasons. The fundamental reason for upholding the State laws prohibiting physician-assisted suicide was "that Anglo-American common law has punished or otherwise disapproved of assisting suicide for over 700 years".127
The opinion of the Court was written by Chief Justice Rehnquist, who wrote,
Next, the State has an interest in protecting vulnerable groups—including the poor, the elderly, and disabled persons—from abuse, neglect, and mistakes... . We have recognized... the real risk of subtle coercion and undue influence in end of life situations.128
Rehnquist, CJ quoted with approval a New York State Task Force Report which said,
Legalizing physician assisted suicide would pose profound risks to many individuals who are ill and vulnerable.... The risk of harm is greatest for the many individuals in our society whose autonomy and well being are already compromised by poverty, lack of access to good medical care, advanced age, or membership in a stigmatized social group.129
Rehnquist, CJ went on to say,
The State's interest here goes beyond protecting the vulnerable from coercion; it extends to protecting disabled and terminally ill people from prejudice, negative and inaccurate stereotypes, and societal indifference.... The State's assisted suicide ban reflects and reinforces its policy that the lives of terminally ill, disabled, and elderly people must be no less valued than the lives of the young and healthy, and that a seriously disabled person's suicidal impulses should be interpreted and treated the same way as anyone else's.130
In other words, a legislatively enforced universal policy of suicide prevention is an essential safeguard against descending into the practice of suicide facilitation with respect to devalued persons.
The U.S. Supreme Court was helped in reaching its decision by a strong intervention as Amici Curiae ("Friends of the Court") by the disability advocacy organizations Not Dead Yet and American Disabled for Attendant Programs Today (ADAPT). The interveners alleged that "no safeguards can be trusted to contain the torrent of discrimination that will be unleashed by lifting the ban on assisted suicide". Neither confining assisted suicide to persons who are terminally ill nor to those who make voluntary requests, argued the interveners, would protect people with disabilities from assisted suicide abuse.131
The intervenors maintained,
As long as people with disabilities are treated as unwelcome and costly burdens on society, assisted suicide is not voluntary but is a forced "choice." Amici are profoundly disturbed by the finding of a constitutional right for assisted suicide in a society which refuses to find a right to adequate and appropriate health care to stay alive. Until society is committed to providing life supports, including in-home personal assistance services, health care, and technological supports, then there is not voluntary choice.... Without the professional commitment to help make living worthwhile for people with disabilities, which is the core of suicide prevention, people with disabilities will not receive the support necessary for informed and voluntary decisions.132
Contained in these strong words pleading for the preservation of State laws prohibiting assisted suicide are safeguards that must be in place if ever those laws are changed, whether in the United States or anywhere else in the world. But they are safeguards that are extremely difficult to create and maintain over time: excellence in health care and personal assistance, universally available to everyone who needs them.
It must be pointed out that the unanimous U.S. Supreme Court decisions in Glucksberg and Vacco only ruled that State laws prohibiting assisted suicide are constitutionally valid. The Court has not ruled on the validity of the Oregon statute, the Death with Dignity Act, which permits physicians to assist in the death of their patients, although a constitutional challenge was mounted by opponents of assisted suicide. The Supreme Court denied the petition of the opponents to review the constitutionality of the legislation.133
The U.S. District Court held that the Death with Dignity Act, the first and only State law to legally authorize physician-assisted suicide, violated the Equal Protection Clause because the safeguards were insufficient to protect the rights of terminally ill patients who may seek assistance in dying. The Ninth Circuit Court of Appeals overturned that ruling when it found that the plaintiffs had no legal standing to challenge the statute because they failed to show any threat of immediate harm and that their claim rested upon a "chain of speculative contingencies."134 The U.S. Supreme Court refused to hear an appeal from that decision, which was on the procedural issue of the standing of the plaintiffs to challenge the law, rather than on the substantive issue of the constitutionality of the Death with Dignity Act.
It should also be noted that neither of the two U.S. Supreme Court cases (Vacco and Glucksberg) involved the criminal prosecution of a physician (like Dr. Jack Kevorkian) who had assisted a patient in dying. The cases were, like Rodriguez in Canada, in the nature of references to the courts for rulings on whether the statutory prohibitions on assisted suicide had to be obeyed.
Justice O'Connor, in her concurring judgment that the New York and Washington State laws were valid, anticipated that at least some States would follow Oregon's example, and that the conflicting concerns about relieving severe end-of-life suffering on the one hand, and protecting the lives and well-being of vulnerable persons on the other, would work themselves out:
There is no reason to think the democratic process will not strike the proper balance between the interests of terminally ill, mentally competent individuals who would seek to end their suffering and the State's interests in protecting those who might seek to end life mistakenly or under pressure.... [T]he challenging task of crafting appropriate procedures for safeguarding... liberty interests is entrusted to the 'laboratory' of the States.135
Further, as Larry Gostin has pointed out, the U.S. Supreme Court clarified in Glucksberg and Vacco that "a physician could engage aggressively in palliation of pain, knowing that a possible, perhaps likely, result was the patient's death".136 This principle, too, was enunciated by Justice O'Connor:
A patient who is suffering from a terminal illness and who is experiencing great pain has no legal barriers to obtaining medication, from qualified physicians, even to the point of causing unconsciousness and hastening death.137
More recent litigation in at least one State court has essentially followed the Supreme Court's lead in refusing to strike down legislation banning assisted death. This case was based on a specific right of privacy contained in Alaska's State Constitution. Judge Eric Sanders found that the state's obligation to ensure "the preservation of human life and the protection of vulnerable individuals" outweighs any person's right to decide to end his or her life.138 If there is a privacy right to assisted death, Sanders J. ruled, that right must be set aside when a more demanding public interest is at stake:
... [O]ne aspect of a private matter is that it is private, that is, that it does not adversely affect persons beyond the actor, and hence is none of their business. When a matter does affect the public, directly or indirectly, it loses its wholly private character, and can be made to yield when an appropriate public need is demonstrated.... The state's assisted suicide ban reflects and reinforces its policy that the lives of terminally ill, disabled, and elderly people must be no less valued than the lives of the young and healthy, and that a seriously disabled person's suicidal impulses should be interrupted and treated the same way as anyone else's.139
Next we turn to the one State in the U.S., Oregon, that has adopted legislation to facilitate physician-assisted suicide.
B. Oregon's Death with Dignity Act
In November, 1994, a "citizens' initiative" enacted the Death with Dignity Act140 in the State of Oregon. This initiative was by ballot, and it passed by the narrowest of margins: 51% in favour and 49% opposed. Its passage was followed by lengthy court proceedings challenging its validity, including a petition that was denied by the U.S. Supreme Court. The legislation finally cleared these judicial obstacles and came into effect on October 27, 1997. There was a further question on the ballot to confirm the legislation the following month, and it passed by a margin of 60% to 40%.141
The Death with Dignity Act "allows terminally ill Oregon residents to obtain from their physicians and use prescriptions for self-administered, lethal medications".142 The Act states that ending one's life in accordance with the law "shall not, for any purpose, constitute suicide, assisted suicide, mercy killing or homicide under the law".143 In order to take advantage of the provisions of the Act, an individual must be at least 18 years old, "capable,. .. determined by the attending physician and consulting physician to be suffering from a terminal disease, and (have) voluntarily expressed his or her wish to die". "Terminal disease" is defined as "an incurable and irreversible disease that has been medically confirmed and will, within reasonable medical judgment, produce death within six (6) months)".144 Such a person "may make a written request for medication for the purpose of ending his or her life in a humane and dignified manner in accordance with this Act".145
The written request must be witnessed by two persons, one of whom must be neither a relative of the patient, a beneficiary of the patient's estate, nor have any connection with the health care facility where the patient resides or is being treated. The patient's attending physician cannot be a witness, but those who are living in a "long term care facility" must have their request witnessed by "an individual designated by the facility".146
Section 3 of the Death with Dignity Act is headed "Safeguards". Such safeguards consist of specified responsibilities of the attending physician and a consulting physician. The attending physician is to determine "whether a patient has a terminal disease, is capable, and has made the request voluntarily".147 Section 3.01 also requires the attending physician to see that the patient is properly informed about his or her diagnosis and prognosis, about potential risks and the probable result of taking the lethal medication, and about "feasible alternatives, including, but not limited to, comfort care, hospice care and pain control". The attending physician must also refer the patient to a "consulting physician", and "for counselling if appropriate". The legislation states that it is not only appropriate, but mandatory, that the patient be referred to a counsellor if either physician is of the opinion that his or her mental state may be affecting his or her ability to make a well-reasoned decision about the request for aid in dying. The purpose of the counselling referral is to determine "whether the patient is suffering from a psychiatric or psychological disorder, or depression causing impaired judgment".148
The request for medication to end the patient's life must be made orally, then in writing, and again orally immediately before the prescription for the lethal medication is written, which cannot be less than 15 days after the initial oral request is made. The patient must be told by the attending physician that he or she can rescind the request at any time, and must be specifically reminded of this right to change his or her mind at the end of the 15-day waiting period, just before the prescription is written. There is also a mandatory 48-hour waiting period from the time the written request is signed, in the event that these 48 hours do not fall within the 15-day waiting period.
The attending physician is required to ask the patient to inform his or her family of the intention of seeking assistance in dying, but the patient is not required to do so.149 The attending physician also has a number of responsibilities in connection with maintaining the patient's medical record and the filing of documents with the State Registrar, Center for Health Statistics, Oregon Health Division. Full documentation is to be sent to the Health Division "within seven working days" of the writing of the prescription for the lethal medication.150
There is no attempt contemplated in the legislation on the part of the Health Division to ensure that any information is filed until after the prescription has been written, and the patient has died. There is also a duty on the dispensing physician or pharmacist to "file a copy of the dispensing record", either by mail or by electronic mail.151 The "safeguards" identified in the legislation are in reality entirely private before the fact, and not open to public scrutiny after the fact.152
Section 3.11 of the Death with Dignity Act imposes on the Oregon Health Division the duty to conduct an annual review of "a sample of records maintained pursuant to this Act", and to publish "an annual statistical report of information collected under this Act".153 at the time of this writing, these statistical reports were available for the first two years of the operation of the Act. In 1998, 24 prescriptions were written for lethal doses of medication, and 16 persons actually used the drugs to end their lives.154 In 1999, 33 prescriptions were written for lethal doses of medication, and 27 died after ingesting these drugs. The numbers of lethal prescriptions increased to 39 in 2000, and to 44 in 2001, but the numbers who actually ingested the prescribed drugs and died levelled off at 27 in 2000 an dropped to 21 in 2001.155 The assisted deaths represented 6 out of every 10,000 deaths in Oregon in 1998, and 9 out of every 10,000 deaths in 1999.156
When compared to persons who died of the same underlying medical condition, the assisted suicides accounted for 39 out of every 10,000 cancer deaths in 1999, nearly double the 20 out of every 10,000 cancer deaths in 1998. These are relatively insignificant numbers. The population of Oregon is just over 3 million, so comparable figures for Canada could presumably be in the order of ten times higher.
The second annual report on the implementation of the Death with Dignity Act157 provides some detailed analysis of the kinds of persons who requested and received assistance in taking their own lives during the first two years of operation. The median age of such patients was 70 years. "As education increased, so did likelihood of participation".158 Fewer than one in three (31%) received a lethal prescription from the first physician they asked. Follow-up interviews with the prescribing physicians and surviving family members revealed that those who chose to die did so for a variety of reasons. Most cited "loss of control of bodily functions", "loss of autonomy", and "physical suffering", although family members reported that 40% of those who were concerned about pain were not actually suffering pain when they began talking about physician-assisted suicide.159
Thirty-one (72%) of those who were assisted by physicians to commit suicide in Oregon under the Death with Dignity Act during the first two years of its operation had cancer. The rest had either chronic obstructive pulmonary disease (5), amyotrophic lateral sclerosis (4), or one of three other disease categories that each accounted for only one patient. One of these categories was AIDS.160 It appears surprising that in a State with a population of over 3 million, only one AIDS patient would choose legal physician-assisted suicide over a period of two years.
Fifteen (35%) of those who ultimately committed physician-assisted suicide were referred to a counsellor for psychiatric evaluation. Since reports are only filed when a patient actually ends his or her life by lethal drugs, there is no information as to how many such referrals resulted in a finding that the patient was incapable of choosing death due to "impaired judgment" arising from a "psychiatric or psychological disorder".161
The only indicators of disability among those who died in 1998 and 1999 are the physicians' reports of "mobility before death". Only 11 (26%) were reported to have "good" mobility. The others had either "poor" mobility (40%) or "none" (33%).162 To these could be added the majority of those who died whose physicians said they wanted to die because of "decreasing ability to participate in activities that make life enjoyable" (77%) or because of "losing control of bodily functions" (58%).163
In spite of a section specifically labelled "Safeguards", Oregon's Death with Dignity Act essentially leaves everything in the hands of the patient, two physicians, and two witnesses. These are the only persons who have to be satisfied that the criteria set out in the statute (terminal illness, mental capacity of the patient, and voluntariness of the decision) have been met. Physicians who prescribe lethal doses of drugs are required under the Act to file reports, but there are no penalties for those who fail to do so.
The legislation presumes, by repetition of the formula no fewer than 18 times in a six section statute, that its purpose and effect is to enable people "to end their lives in a humane and dignified manner".164 This appears to be the primary matter of concern, rather than whether, in each particular case, standards have actually been met that will ensure that there is no abuse of the legislative authority. Given Oregon's system of enacting legislation by means of a "citizens' initiative" on the ballot at election time, words like "humane and dignified" obviously have considerable voter appeal.
Vulnerable persons are potentially excluded from qualification for death (if their disability is mental in nature) through the process of referral for "counselling" to determine if they are likely to make an "impaired judgment". This adds, in some cases, one other person to the small and very private group that is to determine whether the applicant is entitled to die by means of lethal medication.
According to Herbert Hendin, author of the 1998 book Seduced by Death: Doctors, Patients and Assisted Suicide,165 "In more than half of the 142 cases in Oregon for which physicians provided information about interventions, including 18 of the 29 cases in which patients were given prescriptions for lethal medication... there was not even one palliative intervention".166 Hendin went on to say, "Although two thirds of patients requesting assistance with suicide have been shown to be depressed, only 20 percent of such patients in Oregon were reported by physicians to have symptoms of depression".167 Barry Rosenfeld has also expressed concern that "it is impossible to know the extent to which these requests (for assistance with suicide) were fuelled by depression, which in many cases is treatable".168
These critical assessments of the Oregon experience were in response to a February, 2000 article in the New England Journal of Medicine by Ganzini et al.,169 which had reported favourably on the implementation of the statute. In response to Hendin's accusation that palliative care had not been made available to most of those who requested and obtained assistance with suicide, Ganzini and her colleagues wrote that "19 of 29 (such) patients... received comprehensive palliative-care services through a hospice program before or after the request".170 They also acknowledged "that patients for whom palliative care interventions were made were significantly more likely to change their minds about assisted suicide than those for whom interventions were not made"171
Ganzini, et al., admitted that "the magnitude of the role of depression in requests for legalized assisted suicide requires further study", but they concluded their response with a further defence of the practices in Oregon since the enactment of the Death with Dignity Act:
Our data simply do not support the hypothesis that among patients eligible for assistance with suicide,... vulnerable groups, including mentally ill patients, request assistance with suicide disproportionately or receive lethal prescriptions in place of palliative care.172
Whether such assurances will pass the test of time remains to be seen. To the extent that they are presently reliable, they may be based on an early reluctance to encourage recourse to assisted death, rather than on any built-in safeguards, which, as we have seen, are minimal. Oregon's experiment continues to stir considerable controversy across the United States.
C. U.S. Federal Pain Relief Promotion Bill
On October 27, 1999 a Bill was adopted in the U.S. House of Representatives (chiefly with Republican support) that would ban the use of federally controlled drugs to cause death.173 The purpose of the Bill, which consists of amendments to the Controlled Substances Act and other related federal legislation is stated as "to promote pain management and palliative care without permitting assisted suicide and euthanasia".174
The first operational amendment in the Pain Relief Promotion Bill reads as follows:
For purposes of this Act and any regulations to implement this Act, alleviating pain or discomfort in the usual course of professional practice is a legitimate medical purpose for the dispensing, distributing, or administering of a controlled substance that is consistent with public health and safety, even if the use of such a substance may increase the risk of death. Nothing in this section authorizes intentionally dispensing, distributing, or administering a controlled substance for the purpose of causing death or assisting another person in causing death.175
The second part of the Bill provides for increased education and training programs "on the necessary and legitimate use of controlled substances in pain management and palliative care, and means by which investigation and enforcement actions by law enforcement personnel may accommodate such use".176 Amendments are also proposed to the Public Health Service Act to provide for intensified education programs for "palliative care research and quality", and for "education and training in palliative care".177 For purposes of the Bill, palliative care is defined as follows:
... [T]he term 'palliative care' means the active, total care of patients whose disease or medical condition is not responsive to curative treatment or whose prognosis is limited due to progressive, far-advanced disease. The purpose of such care is to alleviate pain and other distressing symptoms and to enhance the quality of life, not to hasten or postpone death.178
News media and the political debate over the Bill have generally treated it as an attempt to render the Oregon Death with Dignity Act inoperative. Oregon politicians and other opponents of the Bill treated it as a serious invasion by Congress of that State's rights and on citizens' rights to determine their own time and means of death. On April 27, 2000, the U.S. Senate Judiciary Committee approved the Bill by a vote of 10-8.179 Because of procedural moves and the change of the U.S. federal administration after the 2000 presidential election, the Bill was never voted on in the Senate.
Whereas Janet Reno, the Attorney General in the Clinton administration had specifically ordered that federal authorities should not interfere with the implementation of the Oregon statute, the new Attorney General, John Ashcroft, issued a memorandum stating that the use of controlled substances for physician assisted suicide was not a legitimate medical purpose, and was therefore prohibited. Any physician who prescribed lethal drugs for such a purpose were to be deprived of their right to prescribe any medications coming within the scope of the federal Controlled Substances Act. This would have had the effect of nullifying the Oregon Death with Dignity Act, but the United States District Court ordered an injunction barring the implementation of the Ashcroft ruling. That injunction was under appeal at the end of 2002.180
Regardless of how its proponents and opponents have viewed it, the Pain Relief Promotion Bill did have a positive element, in that it would have enhanced both the medical community's willingness and capacity to respond to people's end-of-life needs for the relief of suffering and stress without forcing them to make a premature exit. Opponents argued that its provisions for the enhancement of the use of palliative care medications would have been more than offset by the chilling effect it would have had when physicians contemplated their risk of prosecution for wrongfully contributing to the deaths of their patients by over-prescribing pain control drugs.
D. Netherlands practices and legislation
The Netherlands has been for many years, and remains today, the only country in the world where physician-assisted dying is legally permitted nation-wide. A criminal law amendment bill introduced in August, 1999 and finally passed in April, 2001 finally gave full legitimacy to the practices of "termination of life on request" (i.e. voluntary euthanasia) and "assistance with suicide", which have been openly tolerated by the courts and prosecutors in Holland for roughly twenty years. The amendment to the Netherlands Criminal Code, referred to as a "Bill for 'review of cases of termination of life on request and assistance with suicide'"181, does not strictly de-criminalize euthanasia and assisted suicide, but rather legislates what has been the practice of not prosecuting those who commit such acts, provided that prescribed criteria are observed. These acts remain punishable unless "certain criteria of due care are fulfilled", and the physician responsible notifies the municipal coroner.182
The "criteria of due care", which are themselves legislated "in a separate act, namely the Termination of Life on Request and Assistance with Suicide (Review) Act", are as follows:
The physician must:
- be convinced that the patient's request was voluntary, well-considered and lasting;
- be convinced that the patient was facing unremitting and unbearable suffering;
- have informed the patient concerning the latter's situation and prospects;
- have reached the firm conclusion with the patient that there was no reasonable alternative solution to the patient's situation;
- have consulted at least one other independent physician, who has examined the patient and who has formed a judgment concerning the requirements of due care as referred to in a-d above;
- have carried out the termination of life in a medically appropriate fashion.183
The first two and last two of these standards are essentially the same as those in effect for at least the past decade. Only clauses (c) and (d) have been added by the Termination of Life on Request and Assistance with Suicide (Review) Act. At no time has the Netherlands restricted physician assistance in dying to those who are terminally ill, and that criterion is noticeably absent from the above list.
There are five "regional review committees" which have the responsibility for determining whether due care has been observed. The new legislation makes an important change in the role of these review committees. Whereas they have in the past been required to report their findings in every case to the Public Prosecution Service, the new legislation only requires them to do so if they conclude that the criteria of due care have not been fulfilled.184 This in effect will remove a significant safeguard. A final decision about whether the law appears to have been violated is now, in most cases, no longer up to the agency responsible for the enforcement of the law.
The new Dutch legislation also allows children as young as twelve years to request their own death. According to the Justice Ministry Fact Sheet,
In the case of children aged between 12 and 16 the consent of the parents or guardian is required. But in the event of the refusal by one or both parents or the guardian a minor's request may nevertheless be met if the physician is convinced that this would prevent serious harm to the patient.185
Doctors are permitted to act upon advance directives requesting physician assistance in dying, known as "euthanasia declarations", "unless they have good reason not to do so".186
There has been a long history of the development of tolerance for physician assistance in dying in Holland. Euthanasia societies were formed in the early 1970's. In 1981 a Rotterdam court stated the conditions under which aiding suicide and administering voluntary euthanasia would not lead to prosecution. These rules were affirmed by the Supreme Court of the Netherlands in 1984. In 1990 a notification procedure was agreed between the Royal Dutch Medical Association and the Ministry of Justice. 187
Also in 1990, the Government of the Netherlands set up the Remmelink Commission to investigate the actual practices of physicians in bringing their patient's lives to an end. The Commission reported on the numbers of such deaths in 1990 B before the mandatory reporting system was adopted. Nearly one in five deaths in the Netherlands that year were attributable to the actions of physicians, although most of those deaths were through the administration of drugs with the alleged primary intention of alleviating pain. Another 17.5% of all deaths occurred because of the withdrawal or withholding of medical treatment.
Active euthanasia was the cause of far more deaths than was assisted suicide. 2,190, or 1.7% of all deaths in Holland in 1990 were by lethal injection at the request of patients. By comparison, only 258, or 0.2% opted for doctor-assisted suicide. Another 1,030 were given lethal injections without having requested euthanasia.188 About the same number were denied life-sustaining medical treatment without being asked for their consent. The Mennonite Brethren Herald pointed out that, in 1990, 2,150 Dutch citizens who were mentally capable of making a life or death decision had their lives shortened, either by active or passive euthanasia, without being given an opportunity to participate in the decision.189
Although "unremitting and unbearable suffering" has always been and will continue to be one of the necessary pre-conditions for legalized euthanasia in Holland, the 1990 Remmelink Report revealed that in only six percent of all euthanasia cases had the patient listed pain as the only reason for requesting assistance in dying, and in fact pain had only been mentioned by 46 percent of the patients who had died. The most common reason was "loss of dignity" (57 percent), followed by "unworthy dying" (46 percent), "being dependent on others" (33 percent) and "tiredness of life" (23 percent).190
A follow-up study by the Remmelink Commission in 1995, after the mandatory reporting rules had been in effect for a number of years, produced quite similar results, except that voluntary euthanasia had increased from 1.7% of all deaths in the country to 2.4%. This is an increase of well over one thousand people. There were still close to that number receiving lethal injections without asking for them.191
The Special Committee of the Canadian Senate on Euthanasia and Assisted Suicide conducted a video conference on October 10, 1994 with a number of medical experts from the Netherlands.192 One of these experts was Dr. Gerrit Van der Wal, Medical Inspector of Health in North Holland. Dr. Van der Wal told the Senate Committee that there were about three times as many requests for euthanasia than there are people who were actually assisted to die. He also stated that
... cases in which a physician actively terminates the life of a patient without the patient's explicit request... were substantially wide scale. This was the most shocking result of the Van der Maas [Remmelink] study.... [I]t is estimated that this occurred in more than 1,000 cases per year.... In most instances they were no longer able to express their will competently.193
These discrepancies are indeed startling. Two out of three people who ask to be killed are not, and more than a thousand are killed each year without asking.
The Voluntary Euthanasia Society of Scotland, a group that wants to see euthanasia legalized in their own country, recently reported the following startling facts about the situation in the Netherlands:
It is notable... that most acts of euthanasia are not reported: official studies suggest that only 18 per cent were reported in 1990 and 41 per cent in 1995. Those not reported are generally attributed to death by natural causes on the death certificate.194
A 1997 joint press release from the Dutch Ministry of Justice and the Ministry of Health, Welfare and Sport admitted that "more than half of all cases of medical action to end life are not reported".195 The same press release also claimed that "the social scrutiny of actions to end life has increased". There is a curious incongruity between these two statements. Essentially, what the press release means is, "Where but in our country are the issues of euthanasia so transparent to the public eye that we can say with confidence that most of its instances go unreported, in spite of a law that requires them to be reported?" This view was somewhat substantiated by a research paper published by the Australian Parliamentary Library about the same time which concluded that:
... [T]here really is not a shred of evidence that the frequency of this sort of behaviour is higher in the Netherlands than, for example, in the United States; the only thing that is clear is that more is known about it in the Netherlands.196
Dr. Gerrit Van der Wal suggested the same thing when he addressed the Senate Committee on Euthanasia and Assisted Suicide in October, 1994:
Since it is unlikely that the Netherlands is a world apart, the difference between it and other countries, Canada, for example, is the visibility of this part of Dutch medical practice. It must be maintained that openness and critical investigation are the most important ingredients for the prevention of a slippery slope.197
Subsequent research has more than confirmed Van der Wal's assessment of the situation in at least one country where euthanasia is formally prohibited by law. Khuse and her colleagues compared data gathered in Australia in 1996 and the Netherlands in 1995 and concluded:
Our study shows that Australia had a significantly higher rate of intentional ending of life without the patient's consent, both through the administration of drugs and by withholding or withdrawing treatment, than the Netherlands. Overall, 36.5% of all Australian deaths involved a medical decision either partly or explicitly intended to hasten death or not prolong life, compared with 19.5% of deaths in the Netherlands.... If we classify euthanasia as all cases in which death is intentionally accelerated by a doctor, 30% of all Australian deaths (or 37,000 cases) would be cases of euthanasia. The comparable 1995 figure for the Netherlands was 16.6%.198
As we shall shortly consider, Australia may not be the best example of the countries in the world where euthanasia is unlawful. Nevertheless these data suggest that the Netherlands may indeed not be "a world apart".
Russel Ogden alluded to the extent of interventions to hasten death, even in countries where such practices are prohibited by law, when he appeared on March 28, 2000 before the Canadian Senate subcommittee to review developments since the tabling in June, 1995 of the report "Of Life and Death". Professor Ogden spoke about "new developments within the underground assisted death movement", which he associated chiefly with the HIV-AIDS community:
I call this movement a "deathing counterculture" because its constituents see themselves as providing what they call "deathing services", much the way a midwife or a physician might participate in birthing. This so-called "deathing counterculture" is organized and sophisticated.... This underground movement is virtually unstoppable and it appears to be a growth industry. I have no solutions for you on that. This is an entrepreneurial response to what are seen as barriers to legal medically assisted death. It is an outcome of prohibition. It is characteristic of what we have already seen many times with respect to other taboo behaviours. I raise this because we need to consider the consequences of choosing prohibition and social control of assisted suicide and voluntary euthanasia.199
If we are to believe that essentially the same things are happening to the same numbers of people everywhere in the world, regardless of whether states prohibit or permit doctors to hasten death, then the discussion of how to construct safeguards against abuse takes on a very different tone. The prospect that this may be true must necessarily cause a great deal of consternation for those who are seeking ways in which to prevent the discriminatory resort to physician-assisted death for vulnerable people. Whether euthanasia is broadly and publicly permitted, as in the Netherlands, or whether it is strictly forbidden, as in Canada and the United States (Oregon excepted), it appears that the rules will be massively ignored.
E. Northern Territory of Australia's Rights of the Terminally Ill Act
On July 1, 1996, the Rights of the Terminally Ill Act came into effect in the Northern Territory of Australia, making it the first jurisdiction in the world to formally remove legal barriers to euthanasia and assisted suicide. The legislation allowed physicians to act on the request of patients "of sound mind" to assist in terminating the patient's life. The interpretation section of the Act stated that "assist",
... in relation to the death or proposed death of a patient, includes the prescribing of a substance, the preparation of a substance and the giving of a substance to the patient for self administration, and the administration of a substance to the patient.200
References to this legislation are in the past tense because less than a year after its enactment it was declared to have no force or effect by the Australian National Senate.201
While this legislation authorized both physician-assisted suicide and active euthanasia, it included an extensive list of conditions that had to be satisfied before a doctor could be sure of not incurring civil or criminal liability or professional disciplinary action. Three physicians were required to make judgments of the validity of the patient's request to die. One could be a general practitioner, but another had to be "a specialist in the treatment of the terminal illness from which the patient is suffering". The third doctor was to be a qualified psychiatrist who, in every case, had to confirm "that the patient is not suffering from a treatable clinical depression in respect of the illness".202 There were two "cooling off" periods: seven days from the time a patient asks orally before the patient is permitted to sign a certificate of request for assistance in dying, and 48 hours after the signing of the certificate before the request is finally complied with.
The Australian National Senate, in its Euthanasia Laws Act of 1997, not only rescinded the Northern Territory's Rights of the Terminally Ill Act, but also ensured that no similar legislation could be introduced again:
[T]he power of the Legislative Assembly (of the Northern Territory) conferred by section 6 (of the Northern Territory (Self-Government) Act 1978) in relation to the making of laws does not extend to the making of laws which permit or have the effect of permitting (whether subject to conditions or not) the form of intentional killing of another called euthanasia (which includes mercy killing) or the assisting of a person to terminate his or her life.203
F. Proposed legislation in other countries
In several other jurisdictions, steps have been taken to initiate the process of enacting new legislation which would legalize various forms of physician-assisted death. In some countries, courts have introduced such a process (as occurred in Holland) by finding doctors who have assisted or caused people to die not guilty of criminal offences.204
Although there are no major differences between the proposed legislation in countries like South Africa and Scotland, and the State of California on the one hand, and the actual laws that have been in effect in Oregon and the Northern Territory of Australia on the other, there are some novel features which bear examining. Attention will also be paid to "A Model State Act to Authorize and Regulate Physician-Assisted Suicide" drafted by an American team of doctors, lawyers and academics under the auspices of the Hemlock Society.205
The South African Law Commission presented a report in August 1999 which put forward three options for consideration by the government.206 These include maintaining the existing prohibition of intentional killing, approving assistance in dying on request from terminally ill patients to medical practitioners, and the institution of "a multidisciplinary panel... to consider requests for euthanasia according to set criteria".207 A draft bill, to be known as the "End of Life Decisions Act", includes provisions for implementing both the second and third options.
The Commission adopted a set of governing principles which include the appropriateness in "specified circumstances [of the] cessation of all further medical treatment" of patients who are already clinically dead, the right of competent persons "to refuse any life-sustaining medical treatment", and "prescribing sufficient drugs to control the pain of the patient adequately even though the secondary effect of this conduct may be the shortening of the patient's life". Medical practitioners should also be authorized, according to the Commission, to abide by these principles in accordance with advance directives from the patient or "in accordance with the wishes of the family of the patient or authorized by a court order".208
Some of the particular provisions of the draft legislation include the following: (1) a definition of "terminal illness" to include both inevitable death, combined with "extreme suffering", and "a persistent and irreversible vegetative condition with the result that no meaningful existence is possible for the patient"; (2) administering analgesics or sedatives, either by a physician or a nurse, provided that there is "no intention to kill", "until relief is obtained, even if the secondary effect of this action may be to shorten the life of the patient"; (3) under a set of ten criteria, "by way of administering or providing some or other lethal agent, the medical practitioner shall give effect to the request" of a patient to actively end his or her life.209
Under the heading of "Active Voluntary Euthanasia", the South African Law Commission's draft bill offers an alternative version of s. 5 for consideration by the legislators in which the decision to perform active euthanasia would have to be "approved by an ethics committee constituted for that purpose" to be made up of two medical practitioners, one lawyer, one person who speaks the "home language of the patient", one member of the "multidisciplinary team" and one family member.210
If a physician is to give effect to an advance directive which would likely result in the patient's death, the physician must first be "satisfied that the patient concerned is suffering from a terminal illness and is therefore unable to make or communicate considered decisions concerning his or her medical treatment or the cessation thereof" (emphasis added). This is an unusual provision, in that "terminal illness" does not ordinarily deprive a person of the capacity "to make and communicate considered decisions", unless of course under the second prong of the definition of "terminal illness" referred to above ("a persistent and irreversible vegetative condition").
"The Assisted Suicide Act" is a draft bill produced under the sponsorship of the Voluntary Euthanasia Society of Scotland.211 The draft bill is very brief (three sections and a five- paragraph "Schedule"), and sets out the usual requirements that the individual has made a competent request to die, and is either terminally ill or "in extreme physical or mental suffering". The latter criteria are to be determined by two physicians, one of whom had not been involved in the patient's treatment. The distinctiveness of the draft bill lies in its attention to the typical concerns of lawyers B making sure that "negligence claims... or aspects of contract law such as the impact of a physician assisted suicide on insurance policies" B are taken care of.212 These are safeguards against liability on the part of physicians and of the financial interests of heirs, rather than of vulnerable persons whose deaths may not be voluntary.
The drafters specifically state that they have not attempted to identify safeguards, on the grounds that "any Parliament will wish to debate the fine details.... Hence these minutiae are not included in the original Bill". One of its unique provisions is that "When a person does not die as a result of an act authorized by this statute, unless the person is competent and withdraws the request, a registered medical practitioner remains obligated to assist in that person's death".213 This is darkly reflective of the common law rule that a physician is not obligated to render emergency medical assistance to anyone unless he or she initiates such treatment. Then there is an obligation to continue it. In this case the draft bill would enact what might be called an "if at first you don't succeed" provision. It even extends to "any relative" of the person whose wish to die was not effectively carried out, giving them the right "to sue under the law of tort or delict for any distress occasioned thereby".214
Finally, "A Model State Act to Authorize and Regulate Physician-Assisted Suicide" was published in 1996 by a group of legal and medical academics and practitioners in the Boston area, with the involvement of the pro-euthanasia Hemlock Society.215 The proposed legislation focusses on both "terminal illness" (death likely within six months) and persons suffering from "intractable and unbearable illness", meaning "a bodily disorder that cannot be cured or successfully palliated, and that causes such severe suffering that a patient prefers death".216
The patient's request to die, under the terms of the Model State Act, must be a "reasoned choice based on an understanding of the information that the responsible physician has provided to the patient", and must not be "the result of a distortion of the patient's judgment".217 These requirements would effectively neutralize one another if the information provided by the physician were itself to distort the patient's judgment. The request must have "been made free of undue influence by any person", and repeated twice, "without self-contradiction", with a fourteen-day interval between the two requests. The implementation of the request would have to take place within 72 hours of the second request.218
Section 4 of the Model State Act ("Discussion with Patient and Documentation") is designed to ensure that the responsible physician provides the patient with the essential information required to make a sound judgment. This includes, among other things, "all medical care" that could reasonably be made available to the patient "for the purpose of curing or palliating the patient's illness or alleviating symptoms, including pain and other discomfort", and offering the patient "the opportunity to consult with a social worker" whose training and information might "cause the patient to reconsider his or her request".219 The discussion in which the physician provides the foregoing information to the patient is to be witnessed by two adults, at least one of whom must be totally independent of any relationship with the patient or those involved in the care of the patient.220
Under s. 5 of the Model State Act, a physician who is otherwise prepared to provide the patient with the means to end his or her life must first obtain written opinions, (a) from another physician as to the diagnosis of the patient's condition, and (b) from a "psychiatrist, clinical psychologist or psychiatric social worker" that the patient's judgment is "reasoned", "fully informed", "free of undue influence", and is not distorted "due to clinical depression or any other mental illness".221
When the request is finally implemented and the lethal drugs have been given to the patient, the proposed statute would permit another person who believes that the requirements of the Act have been met (not necessarily the physician), "if the patient so requests", to "be present and assist at the time that the patient makes use of medical means of suicide, provided that the actual use of such means is the knowing, intentional, and voluntary physical act of the patient".222
The Model State Act would stipulate that no physician or health care insurer "may require any individual to request medical means of suicide as a condition of eligibility for service, benefits, or insurance". Like the proposed Scottish legislation, the Act would declare that a suicide under its provisions "shall not be considered suicide for purposes of voiding a policy of insurance on the life of such patient".223
While the cost of medical services to the individual is not a matter of primary concern in Canada because of this country's universal health insurance program, the spectre of the high costs associated with end-of-life care and the possibility that services may at some point be "rationed" because of their scarcity is always present. The drafters of the Model State Act, in the Preamble to the proposed statute, address this issue head-on:
Sometimes treatments or other services will be impracticable because the patient lacks the resources or health insurance necessary to pay for them. Such a situation presents health care providers and patients with a painful ethical dilemma. On the one hand, it seems plainly wrong for a patient to be forced to consider suicide because of a lack of ability to obtain treatments or services that might mitigate his or her condition or circumstances. On the other hand, if there is no way to right this wrong in a particular situation, it seems doubly wrong to deny the patient the medical means of suicide that he or she has requested. We believe that if society fails to meet its moral obligation to provide appropriate health care and other services to all its citizens, it cannot justifiably deny individuals relief from conditions that they find all the more unbearable because of society's moral failure.224
This plea that death should not be denied to those who cannot afford appropriate health care is as grotesque in its own way as Marie-Antoinette's infamous response to the French peasants' lack of bread: "Let them eat cake". Is it not reasonable to ask why a "Model State Act", which is only going to take effect after state legislators debate and vote on it clause-by-clause, could not propose a provision committing the state to pay for medical services (a) which the patient cannot afford, and (b) without which the patient will eventually die after a period of intense suffering? The premise behind the Model State Act drafters' "painful ethical dilemma" is a symptom of what the editor of the New England Journal of Medicine recently described as the "insanity" of the American health care system.225 Scott Fitzgibbon, to reinforce his arguments against the legalization of assisted suicide, has reduced this so-called dilemma to its simplest terms: "If they are so badly off they can always get a physician-assisted suicide".226
The "impracticability" of treatment because of a patient's lack of financial resources or insurance, or for any other reason or combination of reasons, is more likely to be raised with reference to persons with disabilities than anyone else. The assessment that a particular form of life-sustaining treatment is "impracticable" for a person with a disability tends to be made, not just because there is no money to pay for it, but also because it will not "cure" his or her disability. Add those two factors together and the pressure to choose to end one's life can become intense.
VIII. ANALYSIS AND CONCLUSIONS
A. Issues, realities, principles and cautions
The issues surrounding legalized physician-assisted death are extremely complex. It seems self-evident that legalizing the various practices that hasten death will, in and of itself, create unacceptable risks for persons who are vulnerable because of disability. The crucial question is how and to what extent those risks can be reduced. Are those problems better solved by legislated safeguards that apply in all situations, or by guidelines for professional practice that will attempt to identify the best outcome to match the specific facts of each individual set of circumstances? Can both approaches — the general and the particular — be incorporated in a single regulatory scheme?
The foregoing survey of existing and proposed rules in various countries governing physician-assisted death reveals that a system with minimal legislated safeguards will leave many vulnerable persons at risk of losing either their lives or their autonomy over personal life-and-death decisions, or both. It must be stated, however, that published reports do not provide clear documentation of disproportionate numbers of persons with disabilities being assisted to die where assisted death has been legalized. The reports of the first two years' experience with physician-assisted suicide in Oregon do say that about three quarters of those who died had either poor mobility or no mobility. The statistics offer no indication of how long the individuals had lived with these impairments. Also, thirty-five percent of those who died in 1998 and 1999 had been referred for a psychiatric examination. These statistics are indicators that there may be a somewhat greater than average risk of death facing persons with disabilities in jurisdictions where assisted death is legal.
Unfortunately, the published data from countries where assisted death is contrary to the law (which is of necessity anecdotal, since no reporting system can exist without a legalized assisted death system) suggest that a continuation of the rigid prohibition of physician-assisted death will likewise leave many individuals at risk. In fact, people may be even more likely to be helped to die, possibly even without their having expressed a wish to do so, in jurisdictions where such activities are in violation of the law than where they are not.227 As a body, the medical profession remains more or less resolutely opposed to euthanasia and assisted suicide,228 but individual doctors are often prepared to take steps clearly forbidden, both by the law and by professional ethics, whether the rules are rigidly protective of human life or not.
Many people believe, on professional, ethical, religious and/or practical grounds, that the only effective safeguard is to maintain the centuries-old prohibition against intentional killing, because every other safeguard has been proven ineffective.229 Others are equally adamant that the only rule that should be imposed is the best interests of patients as they (the patients) and their doctors perceive those interests to be. Such perceptions cannot be presumed to be free of distortion. Many physicians tend, like other people in positions of economic and social power and prestige, to regard the quality of life of persons with debilitating illnesses or other disabilities as unacceptably poor when compared with their own. The question that is never asked, but to which the answer is always readily at hand, is, "Would I want my life to continue if it had the characteristics of the life of this patient?"230
Patients, too, are conditioned to think of their lives more negatively when it is driven home to them that that is how society's arbiters of what constitutes a "good" life view them. There is, however, ample evidence that persons with disabilities place just as much value on their own lives as anyone else. Other people, and health care providers in particular, "consistently and dramatically underestimate quality of life for their patients, as compared to the assessments which those same patients make of their own lives".231 However, when persons with disabilities find themselves in a situation (as they are likely to have done time and again in their lifetime) where it is apparent that other, "abler" people pity them, discriminate against them, or feel uncomfortable in their presence, their view of the quality of their own lives is often diminished. As Gregor Wolbring has written, "We believe that the majority of death wishes are based on a lack of support and understanding for the individual by society".232
The current range of legal controls over physician-assisted death extends from the law's traditional absolute prohibition of any measures intended to speed up the dying process (other than a valid refusal of consent to treatment), such as we still have in Canada, to the permissive assistance-in-dying approaches that have been legislatively adopted in the Netherlands and Oregon and adopted by prosecutorial tolerance in several other places. In those jurisdictions, as long as a doctor says (and another confirms) that they have observed certain standards, chiefly to conform their actions to the competent wishes of their patients, they have no reason to fear either criminal prosecution or professional discipline. Evidently, in the Netherlands at least, freedom from such fears often leads physicians to ignore the reporting requirement altogether.
The next question is whether there is room between these extremes to map out criteria and procedures which permit assistance in dying, while at the same time incorporating safeguards against abuse, or whether the intervening ground is not ground at all, but a yawning chasm. Since it is the objective of this paper to identify safeguards that can be applied when assistance in dying is legally permitted, it is the questionable middle ground that must be surveyed. While doing so, of course, we have to remind ourselves that whenever a safeguard is identified that has at least the appearance of effectiveness, it will strengthen the hand of those who say that total prohibition of assistance in dying is unreasonable, outdated, and must be abandoned.
B. In what kind of a society might it be safe to legalize assisted death?
There are some primary issues for persons with disabilities, and for citizens in general, that must be addressed before attempting to construct a properly safeguarded system where assistance in dying is permitted. The most critical issue for persons with disabilities is the development of the political will required to see that personal supports and protections against discrimination are sufficiently effective to ensure that the life of any person with a disability is not likely to become intolerable. Those who campaign for legalized assistance in dying constantly use the slogan "death with dignity". The campaign to prevent the abuse of such permissive laws, should they ever be adopted in Canada, must be, first and foremost, to obtain guarantees of "life with dignity" for everyone who has a disability, including the disabilities that ordinarily accompany old age and serious illness.
The two reports emanating from the Canadian Senate have stressed the importance of promoting the quality and availability of palliative care. This is another issue that is obviously a prerequisite to the serious consideration of legalizing assisted death. If as few as five percent of dying Canadians receive optimal palliative care when facing death,233 is it acceptable to introduce legalized assistance in dying? Some would say that it is unconscionable to withhold that option. What they mean is that many in the other 95 percent should be given the chance to grasp at the "solution" of a quick and painless assisted death. If abuses are to be avoided, surely the 95 percent ought to be those whose life while dying is still a life of acceptable quality and comfort. Palliative care will also be discussed in the context of the criteria by which the appropriateness of a request for assistance in dying can be assessed. For now, it is an essential characteristic of a society that cares about its members until the end. Only in such a society is there any chance of safety in considering the legalization of assisted death.
C. Prosecution of health care providers
Health care professionals who disobey the law must pay a price. They deserve to have as much clarification as possible as to the nature of both the "law" and the "price". The cases discussed above in which physicians have faced criminal charges for their actions leading to the death of their patients234 demonstrate that there is either a great deal of uncertainty in this area or a serious disrespect for the rule of law, or both. The Senate Committees, both in 1995 and 2000, and Senator Carstairs in her Private Member's Bill S-2, have identified a concern that there is a lack of clarity in the law with respect to withholding or withdrawing treatment, and in the matter of administering pain-relieving drugs that may have, as a secondary and unintended effect, the shortening of the patient's life.
Although the law governing these matters may not be crystal clear, it is certainly clear enough. None of these activities do or should attract criminal liability if the physician is following the informed wishes of his or her patients, and if the intention is never to inflict death upon them by active means, even self-inflicted. However, if health care providers are genuinely unclear as to what they may and may not do, then it is important to do whatever must be done to rectify that situation. If patients are either over-treated or under-treated because their physicians are fearful for their own protection from prosecution or professional discipline, steps to bring greater clarity to the law and/or to people's understanding of the law must be taken.
Russel Ogden told the Senate Subcommittee reviewing the developments since the Special Senate Committee on Euthanasia and Assisted Suicide report was tabled in 1995 that an "outcome of prohibition" is the development of "backroom" euthanasia services.235 Presumably Ogden would extend that assessment to the effects of any "get tough" policy targetted at physicians.
The Court of Appeal for Ontario in the Genereux case,236 adopted a moderate approach to the punishment of a physician who pleaded guilty to assisting in the suicide of two of his patients. He was sentenced to a two-year term. The Court was concerned that a severe sentence would have an adverse effect on the quality of care comparable patients would receive from their doctors in the future. It is arguable that if Dr. Nancy Morrison had been tried and convicted of first degree murder in the death of her terminally ill patient,237 and had consequently been sentenced to life in prison without being eligible for parole for twenty-five years, that other doctors would be extremely careful that they administer too little, rather than too much, pain-killing and sedating medications to their patients. Mandatory severe punishment does not adequately deter doctors from killing their patients, in part because it deters prosecutors from charging them and juries from convicting them.
But this is not to say that the answer is to introduce so-called "compassionate homicide"or third degree murder into the Criminal Code. These innocuous terms only serve to conceal what would be in effect the murder of a vulnerable person.
D. Procedural safeguards
There is a stark contrast between the procedures that accompany assistance in dying in places where the law now permits it (principally Holland and Oregon), and the procedures that have been proposed in Canada. In Holland and in Oregon (and in the Northern Territory of Australia for a brief period in 1996 and 1997), the patient who expresses a wish to be helped to die only needs to find a physician who is prepared to offer that assistance. The physician must obtain confirmation of the legitimacy of the request from a colleague, and must file a report after the death has occurred. There is no independent "jurying"of whether the request ought to be granted.
In Canada, on the other hand, the courts, the minority of the Special Senate Committee on Euthanasia and Assisted Suicide who were prepared to recommend that euthanasia and assisted suicide be made legal, and the academics who have provided expert testimony in these contexts, have invariably called for a before-the-fact hearing, either by a court or by a specially appointed committee or tribunal. Other than in this country, the only proposal found in this research that includes a hearing before an independent body is an alternative option presented by the South African Law Commission.238
Given the degree of risk that would be faced by persons with disabilities in a regime where assisted death is permitted, some form of judicial or quasi-judicial advance approval seems absolutely essential, especially in the case of mental disability. Given, too, the total departure which the legalization of assisted death represents from the centuries-old commitments of both medicine and law to the preservation of human life, it is inconceivable that anyone would seriously object to such procedural safeguards. The recorded pronouncements of our top judges and other authorities indicate that an independent hearing ought to precede any assisted death, and not just when the person requesting to die has an identifiable disability.
What kind of tribunal would be most appropriate? Chief Justices McEachern of British Columbia and Lamer of Canada, in their respective dissenting judgments in the Rodriguez case,239 both would have assigned the task to the superior court of the jurisdiction in which the patient was living. This is in keeping with the extreme seriousness of the request to have one's life intentionally terminated. The courts are designed and intended to be as free from bias as possible, and to have the greatest expertise in deciding complex and difficult questions. On the other hand, they operate on the basis of the adversarial system, which may not be the most appropriate manner in which to approach life or death issues, often where there are no conflicting views as to the best outcome. In addition, judicial expertise is focussed on legal rights, formal procedural rules, and on the evidence brought before the court at the time of a hearing, rather than on a particular field of learning and experience, such as disability support issues or palliative care. If a quasi-judicial option were chosen, the possibility of judicial review is always available to a party who believes that an error has been made.
If requests for assistance in dying are to be adjudicated by a committee or board appointed for that particular purpose, what should its composition be? Russel Ogden's "Aid-in-Dying Boards" do not have a particularly attractive "ring" to them. They are to be appointed by ministers of health, have a "cross-section of professional backgrounds", and to be selected on the basis of "ethics, liberalism and civil libertarianism".240 The criteria ought to be more particular than that. An ethicist who has not demonstrated a bias against persons with disabilities would perhaps be a good candidate. In the context of high-profile cases such as Dawson and Latimer, several Canadian bioethicists have disqualified themselves on that count.241 Although it has been suggested here that he is one of them, Professor Eike-Henner Kluge offered a helpful suggestion, when he appeared before the Special Senate Committee on Euthanasia and Assisted Suicide in 1995, that "a duly empowered representative of an association for handicapped persons" should sit on an "advisory panel" intended to assist the court in cases where the person whose death was at issue lacked the capacity to request death voluntarily. This suggestion would have been even more helpful if it had identified associations of persons with disabilities, and not just those for such persons. Palliative care specialists and social workers should also be represented on such decision-making boards or committees.
The South African Law Commission's suggestion that such a body include someone who "speaks the home language of the patient" recommends itself not just to societies like South Africa that are made up of many different language groups. Although Canada is such a country, the implications go much further than simply providing an interpreter service between the patient and the decision makers. There is a highly important cultural factor that can perhaps best be recognized through the criterion of language. If the patient is deaf, there would be a need not simply for a sign language interpreter, but also for another deaf person to be a member of the board.
Another public role in relation to physician-assisted death is to receive reports, monitor and inform the public about the cases where death was sought. The administration responsible for the hearing panels could also be responsible for this aspect of the regulatory system. A further role might be to adjudicate cases where there are questions about a patient's capacity or wish to refuse life-sustaining treatment.
It is also important that an advocate be assigned to assist the person whose death is under consideration. This would not necessarily be a lawyer, but could well be a member of an organization dedicated to the well-being of those who have a particular illness or disability or any illness or disability. Patients rights organizations exist in some communities, and should be encouraged to play a role where assisted death is being considered. An advocate may be able to assist the person in his or her dealings with the health care professionals involved, who may not have adequately communicated to the person what options are available besides ending his or her life. Conceivably, the advocate could in some cases help the person decide not to seek death, in which case a hearing would become unnecessary.
The concept of advocacy has to be carefully communicated, not only to individuals and families, but also to institutional and government bureaucracies and to health care professionals. Often the advocate is perceived as an intruder, rather than as a knowledgeable person who is committed to the interests (including the autonomy interests) of the vulnerable person. It is a role which requires both natural gifts of empathy and acquired knowledge and skill. For example, an advocate should be familiar with the law governing consent to medical treatment in the province or territory where he or she lives. For the most part, advocacy is and is likely to remain a voluntary activity, although it is sufficiently important to warrant public expenditure.
E. Criteria: who is qualified to receive assistance in dying?
Even in the Netherlands, there have been for many years "criteria of due care" which physicians are theoretically required to maintain if they wish to avoid prosecution for causing or assisting in the deaths of their patients. Those criteria are as follows:
- the patient must have voluntarily and with consistency chosen to seek death.
- the patient must be "facing unremitting and unbearable suffering".
- at least one other physician must agree that the above criteria have been satisfied.
- the termination of life must have been carried out "in a medically appropriate fashion".242
In the Netherlands, "a medically appropriate fashion" includes both euthanasia and assisted suicide. It must be noted that it is not necessary to have a terminal illness to qualify for physician-assisted death in the Netherlands. The Termination of Life on Request legislation recently adopted by the Dutch Parliament added the following two criteria:
- the patient must be informed of his or her condition and prognosis.
- there must be "no reasonable alternative solution" other than death.
Oregon's Death with Dignity Act only makes assisted suicide available (not active euthanasia), and to be eligible one must have a "terminal disease". Those two differences between Oregon and the Netherlands are reflected in huge differences in the utilization of assisted death. On a per capita basis, Dutch people are nearly thirty times more likely than Oregonians to be assisted in dying by their physicians.
Oregon requires several additional elements for a legal assisted suicide:
- a written request witnessed by two adults, at least one having no personal interest at stake.
- mandatory counselling if either of two doctors thinks the patient may have "impaired judgment".
- a fifteen-day waiting period after the patient first requests assistance in dying, and an additional two days after signing a request for such assistance.
- the physician must ask the patient to notify his or her family of the intention to seek assistance in dying (but the patient does not have to do so).
- the physician must tell the patient that the request for assistance in dying can be revoked at any time.
In both Holland and Oregon, physicians who assist their patients to die are required to report each death to the appropriate authorities, although there is evidence of extensive under-reporting in Holland.243
Chief Justice Lamer, in his dissenting opinion in Rodriguez, set out the minimum requirements for assisted suicide he would have imposed, had the majority not ruled that the Criminal Code prohibition of assisted suicide was constitutional. They begin with the requirement that an application be made to the superior court. From that point on, each requirement is a matter that the court must be satisified has been met. They are essentially the same conditions Chief Justice McEachern of the British Columbia Supreme Court would have imposed. One of the two physicians who inform the court of the person's wish must be a psychiatrist. One of the doctors would have to examine the patient every day from the time she or he first applied to the Court until the assisted suicide is carried out. The two Chief Justices did not require the patient to be terminally ill, but they would have required evidence from the physicians that the applicant is physically unable to commit suicide without assistance, or will become so. The court's permission for the doctor to assist the person to commit suicide would expire in 31 days following the first examination by a psychiatrist.244
Undoubtedly the most comprehensive set of criteria for assistance in dying have been published by National Council on Disability in the United States. Being a comprehensive list, it is also a long one, but it is worth reproducing here:
To effectively limit assisted suicides to appropriate situations and make certain that they do not become a vehicle for fatal discrimination against people with disabilities, such procedures would, at a minimum, have to ensure: that the patient's diagnosis is completely accurate; that the condition of the patient is definitely terminal; that the patient's death is imminent; that there are no available treatments that can save or significantly prolong the patient's life; that the patient is suffering unendurable pain and this pain cannot be controlled by medication or alternative treatments or therapies; that the patient wishes to commit suicide; that the patient's decision is based upon full information about the patient's diagnosis, prognosis, and options and the patient has understood this information; that the patient's desire to die is not a result of temporary dejection resulting from disorientation, adjusting to new limitations, or other causes; that the patient's desire to die is not a result of prejudice, stereotypes, and misinformation about people with disabilities and living with a disability; that the patient's decision to seek suicide is reached only after the patient has received, from knowledgeable disinterested sources, a thorough exploration and explanation of treatment options, rehabilitative techniques, assistive devices, accommodations, etc., for living successfully with the patient's disabilities; that the patient has had the opportunity to meet and talk at length with people living with similar disabilities; that the patient has made the decision to choose suicide freely without being influenced by coercion, harassment, intimidation, or duress; that the patient has requested physician assisted suicide repeatedly over a sufficiently long period of time to ensure that it represents a determined steady conviction to end his or her life; that the patient is unable to commit suicide without the assistance of a physician; and that there is oversight by responsible, objective, disinterested, and impartial authorities who can verify whether or not the foregoing prerequisites to a patient's decision to choose suicide have been satisfied.245
Those who pass scrutiny on all of these criteria will be a select company indeed, which is the object of the exercise for those who have good reason to fear the introduction of legalized assistance in dying. The list clearly does not present itself as a convenient "checklist" that a family doctor could work through in a context like those presently operating in Oregon or the Netherlands. Rather, it is the kind of thorough examination of all the relevant facts that only a hearing board or court can successfully undertake.
Invariably, the criteria that must be met for any form of assistance in dying, regardless of the country or state, include the requirement that the patient has made a competent, informed request, without any coercion. These are no doubt the most problematic of the criteria, especially for persons with disabilities. Disability rights activists and many professionals argue that it is virtually impossible to ensure that a decision in favour of death by a vulnerable person will be free of coercion and undue influence, not only by other individuals who are involved in the person's life, but possibly even more so by circumstances imposed by a society that is not prepared to provide the means of staying alive in dignity and good health.
Whether assisted suicide should be restricted to those who are terminally ill is an inherently problematic question. Doctors have considerable difficulty identifying such illnesses with accuracy when death is still more than a few days away. The "death likely within six months" rule that is applied in Oregon is certainly questionable.
The virtue of a process that involves a hearing before an independent tribunal is that the question, "Why does this person want to die now?" can be carefully addressed. There may be circumstances in which the physical and mental misery associated with a disease that is not necessarily going to take the person's life in the immediate future would be a legitimate answer.
On the issue of waiting periods ("cooling off" periods) between the initial request for assistance in dying and the implementation of that request, once again a tribunal would be better positioned to establish "not before" and "not after" dates, rather than having them established in legislation at a fixed period for everyone.
There are two criteria that are far and away more important than any others, and they absolutely must be established by clear and convincing evidence. Once again, an independent tribunal is likely to be in the best position to be satisfied that these criteria have been met. The first is whether the individual has actually made the decision to request death freely and voluntarily, without necessarily extracting him or her from the context of loving relationships. These are anything but simple matters. As Catherine Frazee asserts,
We need to do much more to challenge the fiction that 'what a person wants' is clear, knowable and absolute. Frankly, among humans, the phenomenon of 'what we want' strikes me as entirely fluid, capricious and transitory, and its articulation is invariably no better than an approximation.246
The second crucial criterion by which to determine that assisted death is an acceptable option is whether every reasonable avenue has been fully explored that would make dying no longer the most attractive prospect, either for the person or those near to her or him. This of course includes pain relief (psychic pain, as much as physical) and all aspects of palliative care, as well as an examination of non-medical issues that impact on the individual's will to live.
F. Conclusion
The crux of the debate over assisted death is the issue of personal autonomy. Those who argue that our existing laws criminalizing assisted suicide and active euthanasia should be relaxed take their stand on the principle that each person deserves, to the extent that it is possible, to be the arbiter of how he or she wishes to approach the end of life. It is assumed that some people would choose to hasten that approach, depending on the severity of their discomfort and/or the certainty of their dying in the very near future. Those on the other side of the debate include many who settle the question in their own minds by asserting that there are values which outweigh personal autonomy, and even personal suffering. Such values may come under the heading of "the sanctity of human life", or, for more secularly minded people, the traditional defence of human life which has characterized both medicine and law for hundreds, even thousands, of years.
For people with disabilities, however, there is a third factor, namely whether "personal autonomy" is a reliable safeguard for those whose lives are devalued because they have disabilities. Particularly (but not only) when the disability is "mental" in nature, there is a reasonable and valid concern that the individual's personal wishes will not determine the outcome in any critical issue. For such persons there is not only the problem of establishing one's own "capacity" to make a decision, but mental disability also tends to lead to greater devaluing of the person's life than is the case where one's disability is only physical in nature.
Outside influences on the decision to consent to the termination of one's own life are rarely so blatant as to be easily identified as "coercion", but they are nevertheless very real and powerful. And that is precisely why it is so difficult to fashion safeguards against abuse in the absence of legal prohibitions of assisted death. Only if the threat of abuse is palpable is it likely that safeguards will be taken seriously.
The thrust of this report is that there are serious risks to persons with disabilities in societies where assisted death is regarded as a solution to the suffering and anxiety that many experience as they near the end of their lives. For most people in that circumstance, assisted death may be regarded as "merciful" because it relieves them of the physical and mental ordeal they would otherwise have to endure. For people with disabilities, however, the "mercy" is often seen in terms of ending a life that is perceived by others to be devoid of value because of the individual's disability, rather than being intolerable for the individual because of pain and suffering. Even in Canada, where the law officially continues to uphold the traditional uncompromising respect for human life, safeguards against resorting to assisted death are seriously wanting. Until it can be convincingly demonstrated that all Canadians enjoy full equality and security of the person, regardless of disability, as guaranteed by the Charter of Rights and Freedoms, then any steps toward legalized assistance in dying should be resisted.
References
Books
Battin, Margaret P., Rosamond Rhodes, and Anita Silvers. Physician Assisted Suicide: Expanding the Debate. New York: Routledge, 1998.
Beauchamp, Tom L., ed. Intending Death: The Ethics of Assisted Suicide and Euthanasia. Englewood Cliffs, N.J.: Prentice Hall, 1996.
Doucet, Hubert, Les promesses du crépuscule: réflexions sur l'euthanasie et l'aide médicale au suicide. Saint-Laurent, Québec: Fides, 1998.
Dworkin, Gerald, R.G. Frey, Sissela Bok, Euthanasia and Physician-Assisted Suicide. New York: Cambridge University Press, 1998.
Dworkin, Ronald. Life's Dominion: An Argument about Abortion, Euthanasia and Individual Freedom. New York: Alfred A. Knopf, 1993.
Emanuel, Linda L., ed., Regulating How We Die: The Ethical, Medical, and Legal Issues Surrounding Physician-Assisted Suicide. Cambridge, Mass.: Harvard University Press, 1998.
Enns, Ruth. A Voice Unheard: The Latimer Case and People With Disabilities, Halifax: Fernwood Press, 1999.
Gallagher, H. By Trust Betrayed: Patients, Physicians, and the License to Kill in the Third Reich. New York: Henry Holt and Company, 1990.
Gentles, Ian., ed. Euthanasia and Assisted Suicide: The Current Debate. Toronto: Stoddart, 1995.
Gomez, Carlos F. Regulating Death: Euthanasia and the Case of the Netherlands. Toronto: Maxwell Macmillan Canada, 1991.
Greenberg, Samuel I. Euthanasia and Assisted Suicide: Psychosocial Issues. Springfield, Ill.: Charles C. Thomas, 1997.
Griffiths, John, Alex Bood, and Heleen Weyers. Euthanasia and Law in the Netherlands. Amsterdam: Amsterdam University Press, 1998.
Hendin, Hubert. Seduced by Death: Doctors, Patients, and Assisted Suicide. New York: W. W. Norton, 1998.
Humber, James F., Robert F. Almeder, and Gregg A. Kasting, eds. Physician-Assisted Death. Totowa, N.J. : Humana Press, 1994.
Humphrey, Derek. Lawful Exit: The Limits of Freedom for Help in Dying. Junction City, Oregon: Norris Lane Press, 1993.
Jamison, Stephen. Final Acts of Love: Families, Friends, and Assisted Dying. New York : G.P. Putnam's Sons, 1995.
Jamison, Stephen. Assisted Suicide: A Decision-Making Guide for Health Professionals. San Francisco: Jossey-Bass, 1997.
Keown, J., ed. Euthanasia Examined: Ethical, Clinical, and Legal Perspectives. Cambridge : Cambridge University Press, 1995.
Kung, Hans, and Walter Jens. A dignified dying: a plea for personal responsibility. London: SCM Press, 1995.
Lussier, Christine, Le consentement de la victime en matière d'infractions contre les personnes. Cowansville, Québec: Éditions Y. Blais, 1999.
Marker, R. Deadly compassion. New York: Avon Books, 1993.
McCormick, Richard A. Killing and Allowing to Die: Is there a Difference? Toronto: Regis College, 1997.
McLean, Sheila and Alison Britton, The Case for Physician Assisted Suicide. London: Pandora, 1997.
McKhann, Charles F., A Time to Die: The Place for Physician Assistance. New Haven, CT: Yale University Press, 1999.
Mullens, Anne. Euthanasia: Dying for Leadership. Toronto: Atkinson Charitable Foundation, 1994.
Mullens, Anne. Timely Death: Considering Our Last Rights. Toronto: A.A. Knopf, 1996
Prado, C.G., & S.J. Taylor, Assisted Suicide: Theory and Practice in Elective Death. Amherst, N.Y.: Humanity Books, 1999.
Research Branch, Library of Parliament. Euthanasia and Assisted Suicide. 1996.
Smith, Wesley J. Forced exit: the slippery slope from assisted suicide to legalized murder. New York: Times Books, 1997.
Sneiderman, Barry and Joseph M. Kaufert, eds. Euthanasia in the Netherlands: a Model for Canada? Winnipeg: Legal Research Institute of the University of Manitoba, 1994.
The Latimer Case: The Reflections of People with Disabilities, Winnipeg: Council of Canadians with Disabilities, December, 1998.
Uhlmann, Michael M., ed. Last Rights?: Assisted Suicide and Euthanasia Debated. Washington, D.C.: Ethics and Public Policy Center, 1998.
Weir, Robert F., ed. Physician-Assisted Suicide. Bloomington: Indiana University Press, 1997.
Willke, J.C., and Frederic Wertham, Assisted Suicide & Euthanasia: Past & Present. Cincinnati, OH : Hayes Pub., 1998.
Woodman, Sue, Last Rights: The Struggle over the Right to Die. New York: Plenum Trade, 1998.
Journal Articles
Aly, G. "The legalization of mercy killings in medical and nursing institutions in Nazi Germany from 1938 until 1941", International Journal of Law And Psychiatry 145 (1984).
Angell, M. "The Supreme Court and physician-assisted suicide — The ultimate right". 336 New England Journal of Medicine 50-53 (1997).
Annas, G.J. "Death by prescription: The Oregon initiative". 331 New England Journal of Medicine, 1240-1243 (1994).
Annas, G.J. "The 'right to die' in America: Sloganeering from Quinlan and Cruzan to Quill and Kevorkian", 34 Duquesne L. Rev. 875-77 (1996).
Batavia, Andrew I. "Disability and physician-assisted suicide". 336 New England Journal of Medicine 1671 (June 1997).
Battin, Margaret. "Voluntary euthanasia and the risk of abuse: can we learn anything from the Netherlands?" 20 Law, Medicine and Health Care 133 (Spring-Summer 1992).
Benrubi, G.I. "Euthanasia: The need for procedural safeguards". 326 New England Journal of Medicine 197-198 (1992).
Berghmans, R.L.P., M.J. Kelleher and P. Cosyns, "Physician assisted suicide: a round table debate", 11 European Psychiatry 4 (1996).
Blake, M. "Physician-assisted suicide: a criminal offence or a patient's right?" 5 Medical Law Review 294-316 (Autumn 1997).
Breitbart, William, et al. "Depression, Hopelessness, and Desire for Hastened Death in Terminally Ill Patients with Cancer". 284 Journal of the American Medical Association 2907 (Dec. 13, 2000).
Brock, Dan W., et al. "Symposium on physician-assisted suicide". 109 Ethics: An International Journal of Social, Political, and Legal Philosophy 519-642 (April, 1999).
Burt, Robert A. "The Supreme Court speaks — not assisted suicide but a constitutional right to palliative care". 337 New England Journal of Medicine 1234-1236 (October 23,1997).
Callahan, D. "The legalization of physician-assisted suicide: Creating a regulatory Potemkin village". 30 University of Richmond Law Review 1-83 (1996).
Callahan, Daniel. "Assisted suicide is a power too far". BioLaw: A Legal and Ethical Reporter on Medicine, Health Care, and Bioengineering. Special Sections, 2(7-8). Frederick, MD: University Publications of America; 1996 July-August: S:125-S:126.
Callahan, S. "A feminist case against euthanasia". 77 Health Progress 21-29 (1996).
Campbell, C.S., and B.-J. Crigger, eds. "Mercy, murder, and morality: perspectives on euthanasia". 19 Hastings Center Report 1-32 (1989).
Canick, Simon M. "Constitutional aspects of physician-assisted suicide after Lee v. Oregon", 23 American Journal of Law & Medicine 69-96 (1997).
Caplan, Arthur L., Lois Snyder, and Kathy Faber-Langendoen. "The role of guidelines in the practice of physician-assisted suicide". 132 Annals of Internal Medicine 476 (March 21, 2000).
Capron, A.M. "At law: Sledding in Oregon". 25 Hastings Center Report 34-35 (1995).
Clark, D.C. "'Rational'suicide and people with terminal conditions or disabilities". 2 Issues in Law and Medicine147, 160-161 (1993).
Conwell, Y. and E.D. Caine, "Rational Suicide and the Right to Die — Reality and Myth," 325 New England Journal of Medicine 1100-03 (1991).
Dickens, Bernard M. "Medically Assisted Death: Nancy B. v. Hôtel-Dieu de Québec". 38 McGill Law Journal 1053 (1993).
Doerflinger, Richard M. "An uncertain future for assisted suicide." 29 Hastings Center Report 52 (January, 1999).
Dworkin, R., T. Nagel, R. Nozick, et al. "Assisted suicide: The philosophers' brief". New York Review, March 27, 1997.
Dworkin, Ronald. "Assisted suicide: What the Court really said". New York Review of Books, September 25, 1997.
Dworkin, Ronald. "Euthanasia, morality, and law" (a response to John Finnis). 31 Loyola of Los Angeles Law Review 1147 (June1998).
Emanuel, Ezekiel J. "Euthanasia: Historical, ethical and empiric perspectives". 154 Archives of Internal Medicine 1890-1901 (Sept 1994).
Emanuel, E.J., et al. "Euthanasia and physician-assisted suicide: Attitudes and experiences of oncology patients, oncologists, and the public". 47 The Lancet 1805 (1996).
Emanuel, Ezekiel, et al. "The practice of euthanasia and physician-assisted suicide in the United States." 280 The Journal of the American Medical Association 507 (August 12, 1998).
Faber-Langendoen, Kathy, and Jason H.T. Karlawish. "Should assisted suicide be only physician assisted?" 132 Annals of Internal Medicine 482 (March 21, 2000).
Fenigsen, Richard. "The Report of the Dutch Governmental Committee on Euthanasia" 7 Issues in Law and Medicine 67-72 (1991).
Finnis, John. "Euthanasia, morality, and law". 31 Loyola of Los Angeles Law Review 1123 (June 1998).
Fitzgibbon, Scott. "The failure of the freedom-based and utilitarian arguments for assisted suicide". 42 American Journal of Jurisprudence 211 (1997).
Fitzgibbon, Scott, and Kwan Lai. "The Model Physician-Assisted Suicide Act and the jurisprudence of death." 13 Issues in Law & Medicine 173-232 (Fall, 1997).
Foley, Kathleen. "The Oregon Report: Don't ask, don't tell." 29 Hastings Center Report 3:37 42 (May 1, 1999).
Freedman, Benjamin. "The Rodriguez case: Sticky questions and slippery answers." 39 McGill Law Journal 644-656 (Oct. 1994).
Ganzini, L., H.D. Nelson, T.A. Schmidt, D.F. Kraemer, M.A. Delorit, and M.A. Lee. "Physicians' experiences with the Oregon Death with Dignity Act". 342 New England Journal of Medicine 557 (February 24, 2000).
Gill, C.J. "Suicide intervention for people with disabilities: A lesson in inequality", 8 Issues in Law & Medicine 37 (1992).
Gilmour, Joan. "Withholding and withdrawing life support from adults at common law." 31 Osgoode Hall Law Journal 473-541 (1994).
Gorman, Daniel. "Active and passive euthanasia: the cases of Drs. Claudio Alberto de la Rocha and Nancy Morrison". 160 Canadian Medical Association Journal 857-60 (March 23, 1999).
Gostin, L.O., and R. Weir. "Life and death choices after Cruzan: Case law and standards of professional conduct". 69 The Millbank Quarterly 143 (1991).
Gostin, Lawrence O. "Drawing a line between killing and letting die: the law, and law reform, on medically assisted dying". 21 Journal of Law, Medicine and Ethics 94 (Spring 1993).
Gostin, L.O. "Deciding life and death in the courtroom: From Quinlan to Cruzan, Glucksberg, and Vacco - A brief history and analysis of constitutional protection of the 'right to die'". 278 Journal of the American Medical Association 1523-8 (1997).
Groenewoud, Johanna H., Paul J. van der Maas, Gerrit van der Wal, Michiel W. Hengeveld, Alfons J. Tholen, Willem J. Schudel, and Agnes van der Heide. "Physician-assisted death in psychiatric practice in the Netherlands". 336 New England Journal of Medicine 1795-1801 (June 19, 1997).
Hendin, H. and G.L. Klerman, Physician Assisted Suicide: The Dangers of Legalization, 150 American Journal of Psychiatry 143-145 (1993).
Hendin, H. "Assisted suicide, euthanasia, and suicide prevention: The implications of the Dutch experience". 25 Suicide and Life-Threatening Behavior 193 (1995).
Hendin, H. "Selling death and dignity". 25 Hastings Center Report 19 (1995).
Herr, Stanley S., et al. "No place to go: Refusal of life-sustaining treatment by competent persons with physical disabilities". 8 Issues in Law and Medicine 3 (1992).
Jochemsen, Henk. "Euthanasia in Holland: An ethical critique of the new law". 20 Journal of Medical Ethics 212, 214-215 (1994).
Journal of Pain and Symptom Management, "Special issue on medical ethics: Physician-assisted suicide and euthanasia". Vol. 6: 279-346 (1991).
Kamisar, Yale. "The future of physician-assisted suicide." 34 Trial 48-53 (July, 1998).
Kamisar, Yale. "On the meaning and impact of the physician-assisted suicide cases". 82 Minnesota Law Review 895-1043 (April, 1998).
Kaveny, M.C. "Assisted suicide, the Supreme Court, and the constitutive function of the law". 27 Hastings Center Report 29-34 (1997).
King, P.J. "Targeting the vulnerable". http://www.ohiolife.org/euth/target.htm. (April, 1996).
Kleinman, A. "Intimations of solidarity? The popular culture responds to assisted suicide". 27 Hastings Center Report 34-36 (1997).
Koch, T. "Living vs. dying 'with dignity': A new perspective on the euthanasia debate". 4 Cambridge Quarterly of Healthcare Ethics 2 (1995).
Latimer, Elizabeth. "Euthanasia, physician-assisted suicide and the ethical care of dying patients" 151 Canadian Medical Association Journal 1133-1136 (October,1994).
Lavery, James V., Bernard M. Dickens, Joseph M. Boyle, and Peter A. Singer. "Bioethics for clinicians: 11. Euthanasia and assisted suicide". 156 Canadian Medical Association Journal 1405-1408 (May 15, 1997).
Leenen, H.J.J. "Dutch Supreme Court about assistance to suicide in the case of severe mental suffering". 1 European Journal of Health Law 377 (1994).
Lester, David. "Psychological issues in euthanasia, suicide and assisted suicide." 52 Journal of Social Issues 51 (Summer 1996).
Lo, Bernard, Karen H. Rothenberg, and Michael Vasko. "Physician-assisted suicide in context: Constitutional, regulatory, and professional challenges". 24 Journal of Law, Medicine & Ethics 181 (Fall, 1996).
Longmore, Paul K. "Elizabeth Bouvia, assisted suicide and social prejudice", 3 Issues in Law & Medicine 141 (1987).
Longmore, Paul K. "Medical decision making and people with disabilities: A clash of cultures". 23 Journal of Law, Medicine and Ethics 82 (1995).
Lynn, J. "Assisted death and physician-assisted suicide". 328 New England Journal of Medicine, 964 (1993).
Lussier, Christiane. "Cinq ans après l'affaire Rodriguez: peut-on aider quelqu'un à mourir?" 24 Queen's Law Journal 361 (Spring, 1999).
Manning, Christopher. "Live and let die: Physician-assisted suicide and the right to die." 9 Harvard Journal of Law & Technology 513 (Summer, 1996).
Miller, Franklin G., Timothy E. Quill, Howard Brody, John G. Fletcher, Lawrence O. Gostin, & Diane E. Meier. "Regulating physician assisted death". 331 New England Journal of Medicine 119-122 (July, 1994).
Miller, Paul Steven. "The Impact of Assisted Suicide on Persons with Disabilities — Is It A Right Without Freedom?". 9 Issues in Law & Medicine 47, 54 (1993).
Miles, Stephen H. "Physician-assisted suicide and the profession's gyrocompass". 25 Hastings Center Report 17 (1995).
Miller, F.G., and H. Brody. "Professional integrity and physician-assisted death". 25 Hastings Center Report 8-17 (1995).
Minnow, Martha. "Which question? Which lie? Reflections on the physician-assisted suicide cases." 1997 Supreme Court Review, pp.1-30.
Muller, M. T., Gerrit Van der Wal et al. "Voluntary active euthanasia and physician-assisted suicide in Dutch nursing homes: Are the requirements for prudent practice properly met?" 42 Journal of the American Geriatrics Society 624-629 (June 1994).
Ogden, Russel. "The right to die: A policy proposal for euthanasia and aid in dying." 20 Canadian Public Policy 1-25 (1994).
Ogilvie, Alan D., and S.G. Potts. "Assisted suicide for depression: the slippery slope in action? Learning from the Dutch experience". [Editorial]. 309 British Medical Journal 492 (August,1994).
Orentlicher, David. "The legalization of physician-assisted suicide." 335 The New England Journal of Medicine 663-667 (August 29, 1996).
Osgood, Nancy J. "Assisted suicide and older people — a deadly combination: Ethical problems in permitting assisted suicide". 10 Issues in Law & Medicine 415-435 (1995).
Peruzzi, Nico, Andrew Canapary, and Bruce Bongar. "Physician-assisted suicide: the role of mental health professionals". 6 Ethics and Behavior 353 (1996).
"Physician-Assisted Death." CMA Policy Summary. 152 Canadian Medical Association Journal 248A-248B (January 1995).
Post, Stephen G. "Physician-assisted suicide in Alzheimer's disease". 45 Journal of the American Geriatrics Society 647 (May, 1997).
Price, D.P.T. "Assisted suicide and refusing medical treatment: linguistics, morals and legal contortions", 4 Medical Law Review 270-299 (Autumn 1996).
Quill, T.E., C.K. Cassel, and D.E. Meier. "Care of the hopelessly ill: Proposed clinical criteria for physician-assisted suicide". 324 New England Journal of Medicine1380-1384 (1992).
Quill. T.E., D.E. Meier, S.D. Block, and J.A. Billings. "The debate over physician-assisted suicide: Empirical data and convergent views". 128 Annals of Internal Medicine 552 (April 1998).
Quill, Timothy. "Physician assisted death: After the U.S. Supreme Court ruling." 75 University of Detroit Mercy Law Review 481-498 (Spring, 1998) (entire issue devoted to articles on doctor-assisted suicide).
Salem, Tania. "Physician-assisted suicide: Promoting autonomy — or medicalizing suicide?" 29 Hastings Center Report 3:30-36 (May 1, 1999).
Sheldon, Tony. "Judges make historical ruling on euthanasia." 300 British Journal of Medicine 2: 7-8 (July 1994).
Slome, Lee R., Thomas F. Mitchell, Edwin Charlebois, Jeffrey Moulton Benevedes, and Donald I. Abrams. "Physician-assisted suicide and patients with human immunodeficiency virus disease". 336 New England Journal of Medicine 417 (Feb. 6,1997).
Sneiderman, Barney. "Euthanasia in the Netherlands: A model for Canada?" 8 Humane Medicine 104-115 (April 1992).
Sneiderman, B. and M. Verhoef. "Patient autonomy and the defence of medical necessity: five Dutch euthanasia cases". 34 Alberta Law Review 374 (1996).
Sneiderman, B. "Latimer, Davis and Doerksen: Mercy killing and assisted suicide on the Op. Ed. page". 25 Manitoba Law Journal 449 (1998).
Snyder, Lois, and Arthur L. Caplan. "Assisted suicide: Finding common ground". 132 Annals of Internal Medicine 468 (March 21, 2000).
Somerville, Margaret. "The song of death: The lyrics of euthanasia." 9 Journal of Contemporary Health Law and Policy 1-76 (1993).
Somerville, Margaret. "Guidelines for Legalized Euthanasia in Canada: A Rejection of a Proposal," 32 Annals, Royal College of Physicians and Surgeons of Canada 8 (February 1999).
"Sounding board - Regulating physician-assisted death." 331 New England Journal of Medicine 119-123 (July 1994).
Stolberg, Sylvia D. "Human dignity and disease, disability, suffering: a philosophical contribution to the euthanasia and assisted suicide debate". 11 Humane Medicine 144 (Nov.,1995).
Sullivan, A.D., K. Hedberg, D.W. Fleming. "Legalized physician-assisted suicide in Oregon — The second year". 342 New England Journal of Medicine 598 (2000).
Sulmasy, Daniel. "Killing and allowing to die: Another look". 26 Journal of Law, Medicine & Ethics 55-64 (Spring, 1998).
The Hastings Center. "Dying well? A colloquy on euthanasia and assisted suicide". 22 Hastings Center Report (1992).
Weinrib, Lorraine Eisenstat. "The body and the body politic: Assisted suicide under the Canadian Charter of Rights and Freedoms". 39 McGill Law Journal 619-644 (1994).
Welie, Jos V.M. "The medical exception: physicians, euthanasia and the Dutch criminal law". 17 Journal of Medicine and Philosophy 419 (August, 1992).
Wesley, P. "Dying safely". 8 Issues in Law and Medicine 467 (1993).
Wooddell, Victor, and Kalman J. Kaplan. "An expanded typology of suicide, assisted suicide, and euthanasia". 36 Omega - The Journal Of Death And Dying 219-226 (May-June 1998).
Woolfrey, J. "What happens now? Oregon and physician-assisted suicide". 28 Hastings Center Report 9-17 (1998).
Wöretshofer, Jürgen, and Matthias Borgers. "The Dutch procedure for mercy killing and assisted suicide by physicians in a national and international perspective", 2 Maastricht Journal of European and Comparative Law 7 (1996).
Young, Ernlé W.D. "Physician-assisted suicide: Where to draw the line?" 9 Cambridge Journal of Healthcare Ethics 407 (2000).
Young, Katherine. "A cross-cultural historical case against planned self-willed death and assisted suicide." McGill Law Journal 657-707 (Oct. 1994)
Cases
Compassion in Dying v. Washington, 79 F.3d 790 (9th Cir. 1996) (See Washington v. Glucksberg, 117 S.Ct. 2258, 138 L.Ed.2d 772 (1997).
Cruzan v. Director, Missouri Dep't of Health, 497 U.S. 261 (1990).
Lee v. Oregon, 869 F. Supp. 1491 (Ore. D. 1994). See also Lee v. Oregon (U.S. Court of Appeals, Ninth Circuit, February 1997.)
Malette v. Shulman (1990) 72 O.R. (2d) 417 (Ont. C.A.).
McKay v. Bergstedt, 801 P.2d 617, 637( Nev. 1990).
Nancy B. v. Hôtel-Dieu de Québec (1992), 86 D.L.R. (4th) 385 (Que. S.C.).
R. v. Brush, O.J. No. 656 Ontario Court of Justice (Provincial Division) Hamilton, Ontario Zabel Prov. J. March 2, 1995.
R. v. De La Rocha Reasons For Sentencing Of The Honourable Mr. Justice S. Loukidelis In Timmins Ontario, April 2, 1993.
R. v. Genereux (1999), 44 O.R. (3d) 339.
Rodriguez v. British Columbia (Attorney General) (1993), 24 C.R. (4th) 281 (S.C.C.).
Sampson & Doe v. State of Alaska, Case No. 3AN-98-112888CI (3rd Sup Ct Sept 9,1999); confirmed by the Supreme Court of the State of Alaska, No. 5474, September 21, 2001.
Vacco, Attorney General of New York, et al. v. Quill et al., 117 S.Ct. 2293 (1997).
Washington v. Glucksberg, 117 S.Ct. 2258, 138 L.Ed.2d 772 (1997).
Legislation
Assembly Committee on Judiciary (California), The Death with Dignity Act, April 15, 1999
Baron, Charles H., Clyde Bergstresser, Dan W. Brock, Garrick F. Cole, Nancy S. Dorfman, Judith A. Johnson, Lowell E. Schnipper, James Vorenberg and Sidney H. Wanzer. "A Model State Act to Authorize and Regulate Physician-Assisted Suicide". 33 Harvard Journal on Legislation 1 (1996).
Bill C-203 (Private Member's Bill -Mr. Wenman) - An Act to amend the Criminal Code of Canada (terminally ill persons). Introduced and read for the first time - May 16, 1991; Placed on the Order of Precedence - May 16, 1991; Designated as a votable item - May 31, 1991; Debated at second reading; Read the second time and referred to Legislative Committee H - September 24, 1991.
Great Britain, House of Commons. Bill 207 - Voluntary Euthanasia: A Bill to enable incurably ill patients to ask for euthanasia and for connected purposes. June 1993.
McLean, Sheila A.M., and Joseph Thomson. The Assisted Suicide Act (Draft Scottish Bill). Glasgow: Institute of Law & Ethics in Medicine. Undated. (http://www.euthanasia.org/ssvbill.html)
Northern Territory of Australia, Rights of the Terminally Ill Act, December, 1997.
The Oregon Death with Dignity Act, Oregon Revised Statute 127.800-127.995 (Available at www.ohd.hr.state.or.us/cdpe/chs/pas/ors.htm).
Voluntary Euthanasia Society of England and Wales. Draft bill on physician assisted suicide. 121 Bulletin of Medical Ethics 19 (Sept.,1996).
Reports, Policy Statements, and Submissions
Amici Curiae Brief of Not Dead Yet and American Disabled for Attendant Programs Today, in Dennis C. Vacco, et al. v. Timothy E. Quill, et al., Supreme Court of the United States, October Term, 1995. (http://www.acils.com/NotDeadYet/amicus1.html).
British Columbia, Ministry of Health. Euthanasia and Physician Assisted Suicide. February 1994.
Burgdorf, Robert L. Assisted Suicide: A Disability Perspective. National Council on Disability Position Paper, March 24, 1997.
Canadian Association for Community Living. Who has the Right? Submission to the Senate Committee on Euthanasia, November, 1994.
Canadian Medical Association Policy Summary, "Joint Statement on Resuscitative Interventions", 151 Canadian Medical Association Journal 8 (1994, updated in 1995).
Canadian Medical Association. Physician-assisted death [policy summary]. CMAJ 1995;152:248A-B.
Cica, Natasha. Euthanasia - The Australian Law in an International Context; "Part I: Passive Voluntary Euthanasia", "Part II: Active Voluntary Euthanasia." Research Papers 3 and 4, Parliamentary Library, Australia, 1996.
Department of Human Services, Oregon Health Division, Center for Disease Prevention and Epidemiology. Oregon's Death with Dignity Act: The Second Year's Experience. February 23, 2000.
Gilmour, Joan M., Karen Capen, Barney Sneiderman and Marja Verhoef. Study Paper on Assisted Suicide, Euthanasia and Foregoing Treatment. Toronto: Ontario Law Reform Commission, 1996.
Law Reform Commission of Canada. Euthanasia, Aiding Suicide and Cessation of Treatment. Report #20, 1983.
New York State Task Force on Life and Law. When Death Is Sought: Assisted Suicide and Euthanasia in the Medical Context. May, 1994.
Senate of Canada. Of Life and Death. Report of the Special Senate Committee on Euthanasia and Assisted Suicide. June, 1995.
Subcommittee to update "Of Life and Death" of the Standing Senate Committee on Social Affairs, Science and Technology. Quality End-of-Life Care: The Right of Every Canadian. Final Report. June 6, 2000. (http://www.parl.gc.ca/36/2/parlbus/commbus/senate/com e/upda e/rep e/repfinjun00 e.htm).
Sobsey, Dick. Euthanasia, Assisted Suicide, & People with Disabilities: A Background Paper Prepared for The Premier's Council on The Status of Persons with Disabilities. September, 1994.
News Reports and Opinion Pieces
Council of Canadians with Disabilities. "Airing views on euthanasia and assisted suicide". Abilities [On-Line] Issue 24. (Fall, 1995). http://www.utirc.utoronto.ca/AdTech/ABILITIES/IssFall95TOC.html
Emanuel, Ezekiel. "Whose right to die?". The Atlantic Monthly, Volume 279, No. 3, pages 73-79, March 1997. (http://www.theatlantic.com/issues/97mar/emanuel/emanuel.htm)
Hentoff, Nat. "Disabled, not dead". 6 Responsive Community 4-6 (Fall1996).
Katz, Stephen. "Doctor assisted suicide — a bad oxymoron and a bad idea". Connecticut Post, April 27, 1998.
Kemp, Evan J. "Could You Please Die Now?: Disabled People Like Me Have Good Reason to Fear the Push for Assisted Suicide," The Washington Post C1 (Jan. 5, 1997).
Knickerbocker, Brad. "Sanctioned euthanasia: lessons from abroad". The Christian Science Monitor, December 3, 1998.
Knickerbocker, Brad. "Doctor-aided suicide: shifting politics". The Christian Science Monitor, September 28, 1999.
Shapiro, Joseph. "Larry McAfee, invisible man: The agonizing fight to prevent legalized 'suicide'", U.S. News &World Rep., Feb.19, 1990, at 59, 60.
Singer, Peter. "Nancy Morrison has suffered enough". Toronto Star, June 9, 1998, page A20.
Stolberg, Sheryl Gay. "Considering the unthinkable: Protocol for assisted suicide." 146 The New York Times, p. A1 (June 11, 1997).
Sobsey, Dick, and Gregor Wolbring. Compassionate Homicide versus Equal Protection: A Disability-Rights Perspective@. (Undated) (http://www.ualberta.ca/~ethics/bb7 3com.htm).
Virtue, David. Dutch Government Legalizes Euthanasia. August 11, 1999. (http://virtuosity.freeservers.com/Virtuosity/AUGUST1999/10August.htm).
Wolbring, Gregor. Why Disability Rights Movements Do Not Support Euthanasia: Safeguards Broken Beyond Repair. (Undated) (http://www.thalidomide.ca/gwolbring/why.html)
* M.A., LL.B., Barrister & Solicitor, Toronto, Ontario.
1 This study of the issues involved in the legalization of physician-assisted death has been undertaken at the request of the Council of Canadians with Disabilities. It has been supported financially by the Canadian Bar Association "Law for the Future Fund". The views expressed here are not necessarily those of either the Council of Canadians with Disabilities or the Canadian Bar Association.
2 Senate of Canada. Of Life and Death. Report of the Special Senate Committee on Euthanasia and Assisted Suicide. 1995.
3 Criminal Code of Canada, R.S.C. 1985, c. C-46, s. 231.
4 The phrase "physician-assisted death" has been chosen as the most appropriate general term for the subject of this paper, since it encompasses all forms of activity on the part of medical practitioners which have as their intended effect the hastening of the death of an individual. It should be noted, however, that it is the position of the Canadian Medical Association that "Canadian physicians should not participate in euthanasia and assisted suicide" (Euthanasia and Assisted Suicide (update 1998), May 9, 1998). CMA also takes the position that "Physician-assisted death... does not include the withholding or withdrawal of inappropriate, futile or unwanted medical treatment or the provision of compassionate palliative care, even when these practices shorten life." (Canadian Medical Association. Physician-assisted death [policy summary], Canadian Medical Association Journal 1995;152:248A-B).
5 Criminal Code, s. 222(1).
6 Criminal Code, s. 241.
7 Nancy B. v. Hôtel-Dieu de Québec (1992), 86 D.L.R. (4th) 385 (Que. S.C.); Ciarlariello v. Schacter [1993] 2 S.C.R. 119.
8 Sulmasy, Daniel. "Killing and allowing to die: Another look". 26 Journal of Law, Medicine & Ethics 55-64 (Spring, 1998); McCormick, Richard A. Killing and Allowing to Die: Is there a Difference? Toronto: Regis College, 1997; Gostin, L.O. "Deciding life and death in the courtroom: From Quinlan to Cruzan, Glucksberg, and Vacco - A brief history and analysis of constitutional protection of the 'right to die'". 278 Journal of the American Medical Association 1523-8 (1997). The Supreme Court of the United States in Vacco v. Quill, 117 Supreme Court Reporter 2293 (1997) found that "the distinction between letting a patient die and making that patient die is important, logical, rational, and well established. It comports with fundamental legal principles of causation... and intent" (Syllabus, p. ii).
9 Dr. Hugh Lafave, personal communication, June 6, 2000; Faber-Langendoen, Kathy, and Jason H.T. Karlawish. "Should assisted suicide be only physician assisted?" 132 Annals of Internal Medicine 482 (March 21, 2000).
10 A full account of the Latimer case can be found in Ruth Enns, A Voice Unheard: The Latimer Case and People With Disabilities, Halifax: Fernwood Press, 1999. For a further disability rights perspective on the case see The Latimer Case: The Reflections of People with Disabilities, Winnipeg: Council of Canadians with Disabilities, December, 1998.
11 Criminal Code, s. 231(2).
12 Criminal Code, s. 745.
13 Canadian Charter of Rights and Freedoms, Part I, Constitution Act, 1982.
14 R. v. Latimer, [2001] 1 S.C.R. 3, para. 86.
15 "Mercy and Latimer a hard sell for prof", Doug Beazley, Edmonton Sun, October 27, 2000.
16 Factum of the Intervener, COPOH in Rodriguez v. British Columbia (Attorney General) [1993] 3 S.C.R. 519.
17 R. v. Genereux (1999), 44 O.R. (3d) 339.
18 Factum of the Council of Canadians with Disabilities in R. v. Genereux. The particulars and outcomes of both the Rodriguez and Genereux cases are discussed in detail below in the text accompanying Notes 68 through 81.
19 See Aly, G. "The legalization of mercy killings in medical and nursing institutions in Nazi Germany from 1938 until 1941", International Journal of Law And Psychiatry 145 (1984) and Gallagher, H. By Trust Betrayed: Patients, Physicians, and the License to Kill in the Third Reich. New York: Henry Holt and Company, 1990.
20 See for example "Retired Austrian doctor on trial for wartime child euthanasia program", The National Post, March 21 and 22, 2000. An 84-year-old former neurologist and psychiatrist was finally charged with murder over the deaths of children in unspeakable "experiments" in which the children were intentionally infected with diseases and left untreated in a Vienna institution in 1944. His case was adjourned because his defence claims that he is unfit to stand trial due to his frailty and dementia. It is ironic that he, like former Chilean dictator Augusto Pinochet, is now judged to be protected from the rigours of a criminal trial because he is disabled, when it was persons with disabilities who were the victims of his alleged crimes.
21 Testimony of Hugh Scher before the Standing Senate Committee on Social Affairs, Science and Technology subcommittee to review developments since the tabling in June 1995 of the final report of the Special Senate Committee on Euthanasia and Assisted Suicide, entitled: "Of Life and Death", March 20, 2000.
22 Note 16 above.
23 See Rodriguez, Note 16 above; Washington v. Glucksberg and Vacco v. Quill, 117 Supreme Court Reporter 2258 and 2293 (1997).
24 Re S.D., [1983] 3 W.W.R. 597 (Provincial Court) and 618 (Supreme Court of B.C.).
25 Ibid., p. 633.
26 Orville R. Endicott, The Right of Persons with Intellectual Handicaps to Receive Medical Treatment. Toronto: Canadian Association for Community Living, 1990, p. 25.
27 For the law pertaining to emergency treatment, see, for example, Ontario's Health Care Consent Act, 1996 Statutes of Ontario, c. 2, Schedule A, s. 25(2).
28 Catherine Frazee, personal communication, October 9, 2000.
29 Canadian Medical Association. Physician-assisted death [policy summary]. Canadian Medical Association Journal 1995; 152:248 A-B.
29 Criminal Code, s. 241.
30 Criminal Code, s. 245.
31 Criminal Code, s. 214.
32 Hugh Scher, Note 21 above.
33 Criminal Code, s. 153.1.
34 Hugh Scher, Note 21 above.
35 Health Care Consent Act, 1996 Statutes of Ontario, c. 2, Schedule A.
36 Ibid., s. 10(1).
37 Ibid., s. 11(1).
38 Ibid., s. 11(3).
39 Ibid., s. 4(1). It is important to note that capacity only applies to a particular treatment - not to any and all treatments. Section 15(1) of the Act states that "a person may be incapable with respect to some treatments and capable with respect to others".
40 Ibid., s. 21(1).
41 Ibid., s. 21(2)(a) and (b) (emphasis added).
42 Ibid., s. 21(2)(c).
43 Ibid., Part V (ss. 70-81).
44 Ibid., s. 32.
45 Ibid., s. 33(1).
46 Ibid., s. 35(1).
47 Ibid., s. 36. It is interesting to note that this provision is based on the optimistic assumption that therapeutic and palliative outcomes will improve over time. This optimism flies in the face of those who are campaigning for the enactment of provisions that would enable people to choose the time and means of their death, since such provisions have the potential to reduce society's concentration on training and research geared to extending life and reducing end-of-life suffering.
48 Ibid., s. 37.
49 [1993] 3 S.C.R. 519.
50 Eldridge v. British Columbia (Attorney General), [1997] 3 S.C.R. 624, para. 56.
51 Law v. Canada (Minister of Employment and Immigration), [1999] 1 S.C.R. 497. The issue in this case was whether it was discrimination on grounds of age for a widow under the age of 35 to be denied survivor benefits under the Canada Pension Plan. The Supreme Court ruled that women under the age of 35 are not a group that s. 15(1) is intended to protect from discrimination, since, as a group, they do not have a history of being disadvantaged.
52 Granovsky v. Minister of Employment and Immigration, Supreme Court of Canada, May 18, 2000, File No. 26615.
53 Ibid., Para. 70.
54 Note 49 above.
55 Note 24 above and accompanying text.
56 Re S.D., [1983] 3 W.W.R. 618, 629-630.
57 Cited in Mary A. Kassian, The Feminist Gospel: The Movement to Unite Feminism with the Church, Wheaton, Illinois: Crossway Books, 1992. This penetrating observation, made by Justice Wilson in a speech at Osgoode Hall Law School in 1990 and treated derisively by Mary Kassian, was brought to the author's attention by Catherine Frazee.
58 Note 7 above.
59 (1990) 72 O.R. (2d) 417 (Ont. C.A.).
60 Ibid., Headnote.
61 Dickens, Bernard M. "Medically assisted death: Nancy B. v. Hôtel-Dieu de Québec". 38 McGill Law Journal 1053 (1993) (Abstract).
63 Gorman, Daniel. "Active and passive euthanasia: the cases of Drs. Claudio Alberto de la Rocha and Nancy Morrison". 160 Canadian Medical Association Journal 857-60 (March 23, 1999).
64 Ontario Court (General Division) Her Majesty The Queen against Alberto De La Rocha. Reasons for sentencing of the Honourable Mr. Justice S. Loukidelis in Timmins, Ontario on the 2nd day of April, 1993.
65 Ibid.
66 Ibid. (emphasis added).
67 Note 55 above and accompanying text.
68 Testimony of Professor Jocelyn Downie, Health Law Institute, Dalhousie University, before the Standing Senate Committee on Social Affairs, Science and Technology subcommittee to review developments since the tabling in June 1995 of the final report of the Special Senate Committee on Euthanasia and Assisted Suicide, entitled:"Of Life and Death", February 14, 2000.
69 R. v. Genereux (1999), 44 O.R. (3d) 339 (Court of Appeal for Ontario).
70 Ibid., pp. 341-342.
71 Ibid.
72 [1993] 3 S.C.R. 519.
73 Ibid., Headnote.
74 Ibid.
75 Ibid.
76 Ibid.
77 Lepofsky, David. "A report card on the Charter's guarantee of equality to persons with disabilities after 10 years — What progress? What prospects?". 7 National Journal of Constitutional Law 263, at 371.
78 Rodriguez, Note 72 above, Headnote.
79 Lepofsky, Note 77 above, pp. 371-372.
80 Rodriguez, Note 72 above, Headnote.
81 Ibid.
82 Catherine Frazee, personal communication, October 9, 2000.
83 Senate of Canada. Of Life and Death. Report of the Special Senate Committee on Euthanasia and Assisted Suicide. 1995.
84 Ibid., pp. ix-x.
85 Ibid., p. xi.
86 Ibid., pp. x & xi.
87 Ibid., p. xi. It has recently been pointed out that this was not a unanimous recommendation, since one member of the Senate Committee, Senator Eymard Corbin, was not present when this recommendation was voted on, and has since stated that he would have voted against it (Presentation by Hugh Scher at a workshop sponsored by the Euthanasia Prevention Coalition of Ontario, April 29, 2000).
88 Ibid., p. 85.
89 Ibid., p. 73.
90 Ibid., pp. 73-74 (emphasis added).
91 Ibid., pp. 56-57.
92 R. v. Rodriguez (1993), 76 B.C.L.R. (2d) 145.
93 Ibid., at 163.
94 Ibid.
95 Of Life and Death, Note 73, pp. A-54-55.
96 Russel Ogden. "The right to die: A policy proposal for euthanasia and aid in dying". 20 Canadian Public Policy — Analyse de Politiques 1 (1994).
97 Of Life and Death, Note 73, p. A-43.
98 Ibid., p. A-43.
99 Ibid.
100 Ibid., pp. A-44 & 45.
101 Ibid., p A-46 (emphasis added).
102 See text at Note 26 above.
103 Subcommittee to update "Of Life and Death" of the Standing Senate Committee on Social Affairs, Science and Technology. Quality End-of-Life Care: The Right of Every Canadian. Final Report. June 6, 2000.
104 Ibid., Part II: Report Card 2000.
105 Ibid., Introduction.
106 Ibid., The Subcommittee's Conclusions.
107 Ibid., Part I, The Need for a National Strategy B Our Priority.
108 Ibid., Part I.B.1.
109 Ibid., Part I.B.5. (emphasis added)
110 Note 91 above.
111 Catherine Frazee, personal communication, October, 2000.
112 Quality End-of-Life Care: The Right of Every Canadian, Note 102 above, Part II.F.
113 Ibid., Part II.C.
114 Canadian Healthcare Association, Canadian Medical Association, Canadian Nurses Association and Catholic Health Association of Canada. "Joint Statement on Resuscitative Interventions" (Update1995), October 1995, and "Joint Statement on Preventing and Resolving Ethical Conflicts Involving Health Care Providers and Persons Receiving Care," 1999.
115 Quality End-of-Life Care, Part II.F.
116 Bill S-2, 2nd Session, 36th Parliament, 48 Elizabeth II, 1999, Preamble. Senator Carstairs was a member of the Senate Committee on Euthanasia and Assisted Suicide and served as the Chair of the Senate Subcommittee to update Of Life and Death.
117 See Note 55 above and accompanying text.
118 See for example the discussion of Ontario's Health Care Consent Act above at Note 35 and following.
119 Euthanasia Prevention Coalition of Ontario, News Release, November 1, 1999.
120 Note 96 above.
121 Ibid., pp. 17-18.
122 Ibid., pp. 18-19.
123 Ibid., pp. 19-20.
124 See Note 101 above and accompanying text.
125 Bouvia v. Superior Court, 225 Cal. Rptr. 297 (Ct. App. 1986); State v. McAfee, 385 S.E. 2d 651 (Ga. 1989); In re Rivlin (Mich. Cir. Ct. 1989) (No. 89369904).
126 Washington v. Glucksberg and Vacco v. Quill, 117 Supreme Court Reporter 2258 and 2293 (1997).
127 Washington v. Glucksberg, Syllabus, p. i.
128 Ibid.
129 New York State Task Force on Life and Law. When Death Is Sought: Assisted Suicide and Euthanasia in the Medical Context (1994), p. 120.
130 Washington v. Glucksberg
131 Amici Curiae Brief of Not Dead Yet and American Disabled for Attendant Programs Today in Vacco v. Quill.
132 Ibid.
133 Oregon Health Division's Center for Health Statistics and Vital Records, http://www.ohd.hr.state.or.us/chs/pas/pas.htm. The Oregon legislation is dealt with in detail below at Note 140 and following.
134 Lee v. Oregon (U.S. Court of Appeals, Ninth Circuit, February 1997.)
135 Vacco v. Quill, 2293.
136 Gostin, L.O. "Deciding life and death in the courtroom: From Quinlan to Cruzan, Glucksberg, and Vacco - A brief history and analysis of constitutional protection of the 'right to die'". 278 Journal of the American Medical Association 1523-8 (1997), at 1527.
137 Washington v. Glucksberg, 2258.
138 Sampson & Doe v. State of Alaska, Case No. 3AN-98-112888CI (3rd Sup. Ct., Sept 9,1999).
139 Ibid., pp 8-10.
140 Oregon Death with Dignity Act. Oregon Revised Statute 127.800-127.995. (Available at www.ohd.hr.state.or.us/cdpe/chs/pas/ors.htm).
141 "Oregon's Death with Dignity Act". Oregon Health Division's Center for Health Statistics and Vital Records, http://www.ohd.hr.state.or.us/chs/pas/pas.htm.
142 Ibid.
143 Death with Dignity Act, s. 3.14. It is interesting to note that, in spite of this statutory disclaimer, the Oregon Health Division, in its Annual Report for 1999, refers to the legislation as "allowing legal physician-assisted suicide" ("Oregon's Death with Dignity Act: the Second Year's Experience", Summary, http://www.ohd.hr.state.or.us/chs/pas/ar-smmry.htm.).
144 Death with Dignity Act., s. 1.01(12).
145 Ibid, s. 2.01.
146 Ibid., s. 2.02.
147 Ibid., s. 3.01.
148 Ibid., s. 1.01.
149 Ibid., s. 3.05.
150 Reporting Requirements of the Oregon Death with Dignity Act, s. 333-009-0100 (Reporting), http://www.ohd.hr.state.or.us/chs/pas/oars.htm..
151 Ibid.
152 Death with Dignity Act, s. 3.11(2).
153 Ibid., s. 3.11 (1) and (3).
154 "Oregon's Death with Dignity Act: the Second Year's Experience", Summary, p. 1 (http://www.ohd.hr.state.or.us/chs/pas/ar-smmry.htm).
155 Oregon Public Health Services News Release, Feb. 6, 2002.
156 Ibid., p. 2.
157 Department of Human Services, Oregon Health Division, Center for Disease Prevention and Epidemiology. Oregon's Death with Dignity Act: The Second Year's Experience. February 23, 2000, (http://www.ohd.hr.state.or.us/chs/pas/99pasrpt.pdf); also published as Sullivan, A.D., K. Hedberg, D.W. Fleming. "Legalized physician-assisted suicide in Oregon — The second year". 342 New England Journal of Medicine 598 (2000).
158 Ibid., p. 10.
159 Ibid., p. 11.
160 Ibid., Table 1.
161 Death with Dignity Act, s. 1.01(4).
162 Oregon's Death with Dignity Act: The Second Year's Experience, Table 1.
163 Ibid., Table 2.
164 Death with Dignity Act, ss. 1.01(7), 1.01(11), 2, 2.01, 3.01(9), 3.03, 3.04, 3.06, 3.09(1), 3.09(2), 3.12(1), 3.12(2), 3.13 (twice), 4.01(1), 4.01(4), 6.01 (twice) (emphasis added).
165 Hendin, Hubert. Seduced by Death: Doctors, Patients, and Assisted Suicide. New York: W. W. Norton, 1998.
166 Herbert Hendin, Letter to the Editor, 343 New England Journal of Medicine, July 13, 2000.
167 Ibid.
168 Barry Rosenfeld, Letter to the Editor, 343 New England Journal of Medicine, July 13, 2000.
169 Ganzini, L., H.D. Nelson, T.A. Schmidt, D.F. Kraemer, M.A. Delorit, and M.A. Lee. "Physicians' experiences with the Oregon Death with Dignity Act". 342 New England Journal of Medicine 557 (February 24, 2000).
170 Linda Ganzini, Melinda Lee and Terri Schmidt, Letter to the Editor, 343 New England Journal of Medicine, July 13, 2000. It is unclear how Ganzini, et al. and Hendin could have differed so markedly in their interpretation of the data.
171 Ibid.
172 Ibid.
173 Pain Relief Promotion Act (S 1272, HR 2260).
174 Ibid.
175 Ibid., s. 101.
176 Ibid., s. 102.
177 Ibid., ss. 201 and 202.
178 Ibid.,
179 "Pain relief bill passes panel", The Oregonian, Friday, April 28, 2000.
180 "US Gov't Challenges Oregon Assisted Suicide Law", Reuters Health, September 23, 2002.
181 "Fact Sheet: Termination of life on request and assistance with suicide", Netherlands Ministry of Justice, May 9, 2000. (http://www.minjust.nl:8080/a_beleid/fact/suicide.htm).
182 Ibid.
183 Ibid.
184 Ibid.
185 Ibid. There were reports that the provision making euthanasia available to children as young as twelve years would be dropped (eg. Pro-Life Infonet, http://euthanasia.com/neth99.html), but this was not the case.
186 Ibid.
187 Voluntary Euthanasia Society of Scotland, "Euthanasia in Holland", http://www.euthanasia.org/dutch.html#remm
188 Ibid.
189 Mennonite Brethren Herald, "The Dutch 'Model'", Vol. 35, No. 8 (undated) (http://www.mbconf.ca/mb/mbh3508, dutch.htm)
190 Department of the Parliamentary Library. Euthanasia - the Australian Law in an International Context. Research Paper 4, 1996-97 (http://www.aph.gov.au/library/pubs/rp/1996-97rp4.htm).
191 "Euthanasia in Holland", Note 186 above.
192 Video Conference: Ottawa and Utrecht: Part I, October 25, 1994. (http://www.islandnet.com/deathnet/video_conf.html.)
193 Ibid.
194 "Euthanasia in Holland", Note 186 above.
195 "Review of euthanasia cases to be brought more into line with medical practice", Press Release from the Netherlands Ministry of Justice and Ministry of Health, Welfare and Sport, Jan. 21, 1997 (emphasis added).
196 Euthanasia - the Australian Law in an International Context, Note 186 above.
197 Video Conference: Ottawa and Utrecht, Note 188 above.
198 Kuhse, Helga, Peter Singer, Peter Baume, Malcolm Clark and Maurice Rickard. "End-of-life decisions in Australian medical practice". An article published on the Internet by The Medical Journal of Australia, 1997 http://www.mja.com.au/.
199 Testimony of Russel Ogden before the Standing Senate Committee on Social Affairs, Science and Technology subcommittee to review developments since the tabling in June, 1995 of the final report of the Special Senate Committee on Euthanasia and Assisted Suicide, entitled: "Of Life and Death", March 28, 2000.
200 Rights of the Terminally Ill Act 1995 (NT), s. 3.
201 Euthanasia Laws Act 1997, No. 17 of 1997, s. 3, Schedule 1, proclaimed on March 24, 1997.
202 Euthanasia - the Australian Law in an International Context, Note 189 above.
203 Euthanasia Laws Act 1997, Note 200 above, Schedule 1, subs. (1).
204 For example, Colombia ("Euthanasia and Assisted Suicide Outside the U.S.", http://www.religioustolerance.org/euth_wld.htm) and Switzerland, where "the legal system has condoned the practice for sixty years" ("The Practice of Assisted Suicide in Switzerland", http://www.finalexit.org/pract swiss.html).
205 Baron, Charles H., Clyde Bergstresser, Dan W. Brock, Garrick F. Cole, Nancy S. Dorfman, Judith A. Johnson, Lowell E. Schnipper, James Vorenberg and Sidney H. Wanzer. "A Model State Act to Authorize and Regulate Physician-Assisted Suicide". 33 Harvard Journal on Legislation 1 (1996).
206 African Law Commission. Report on Euthanasia and the Artificial Preservation of Life. August, 1999 (http://www.law.wits.ac.za/salc/report/euthansum.html).
207 Ibid., Summary of Recommendations.
208 Ibid.
209 Report on Euthanasia and the Artificial Preservation of Life, draft End of Life Decisions Act, ss. 1(1), 4(1) and 5(1) (emphasis added). In spite of the mandatory wording in s. 5(1), it should be pointed out that s. 10 of the draft bill excuses a medical practitioner from doing "anything that would be in conflict with his or her conscience or any ethical code to which he or she feels himself or herself bound".
210 Ibid.
211 McLean, Sheila A.M., and Joseph Thomson. The Assisted Suicide Act (Draft Scottish Bill). Glasgow: Institute of Law & Ethics in Medicine. Undated. (http://www.euthanasia.org/ssvbill.html)
212 Ibid.
213 Ibid., Schedule, para. 3.
214 Ibid., para. 5.
215 "A Model State Act to Authorize and Regulate Physician-Assisted Suicide", Note 204 above.
216 Ibid., s. 2 (i) and (d).
217 Ibid., s. 3(a)(3)(B) and (A).
218 Ibid., s. 3(a)(3)(C) and (D).
219 Ibid., s. 4(a) and (b).
220 Ibid., s. 4(D)(1).
221 Ibid., s. 5(a) and (b).
222 Ibid., s. 7(a) (emphasis added).
223 Ibid., s. 12(a) and (b).
224 "A Model State Act to Authorize and Regulate Physician-Assisted Suicide", Note 204 above, Preamble (emphasis added) (http://www.rights.org/~deathnet/MSA_preamble.html).
225 Marcia Angell, addressing the Annual General Meeting of the British Columbia Medical Association and Pacific International Medical Congress 2000, Victoria, B.C., July 1, 2000.
226 Fitzgibbon, Scott. "The failure of the freedom-based and utilitarian arguments for assisted suicide". 42 American Journal of Jurisprudence 211, at 260 (1997).
227 See Note 198 above, and accompanying text.
228 See, for example, Canadian Medical Association. Physician-assisted death [policy summary]. CMAJ 1995;152:248A-B.
229 Wolbring, Gregor. Why Disability Rights Movements Do Not Support Euthanasia: Safeguards Broken Beyond Repair. (Undated) (http://www.thalidomide.ca/gwolbring/why.html)
230 Interestingly, many laws in jurisdictions where assisted death is permitted, and likewise draft laws where it is proposed, stipulate a process to determine whether a candidate for death has a mental condition that would cause him or her to have "impaired judgment" in considering whether to request assistance in dying. Never is it suggested that the health practitioner on whose information they must rely in reaching their decision might also suffer from "impaired judgment".
231 Catherine Frazee, Speaking Notes, Canadian HIV/AIDS Skills Building Symposium, Panel on End of Life Decisions, January 16, 1998.
232 Note 228 above, p. 11.
233 See Note 107 above.
234 See Notes 62 through 71 above.
235 See Note 198 above.
236 See Notes 68 to 71 above and accompanying text.
237 See Note 67 above and accompanying text. See also Singer, Peter. "Nancy Morrison has suffered enough". Toronto Star, June 9, 1998, page A20.
238 See Note 205 above.
239 See Notes 72 and 91 above.
240 See Notes 96 and 120 and accompanying text.
241 See, for example, Note 26 above.
242 See Note 180 above.
243 See Note 193 above.
244 See Note 81 above.
245 Burgdorf, Robert L. Assisted Suicide: A Disability Perspective. National Council on Disability Position Paper, March 24, 1997, p. 23 (http://www.ncd.gov/newsroom/publications/suicide.html).
246 Catherine Frazee, personal communication, October 9, 2000.
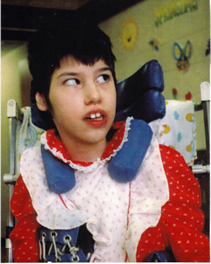
Tracy Latimer
The Latimer Case
The Latimer case directly concerned the rights of persons with disabilities. Mr. Latimer's view was that a parent has the right to kill a child with a disability if that parent decides the child's quality of life no longer warrants its continuation. CCD explained to the court and to the public how that view threatens the lives of people with disabilities and is deeply offensive to fundamental constitutional values. Learn more.
