Act Now

Empower U: Learn to Access Your Disability Rights Training on Canadian Human Rights, the Convention on the Rights of Persons with Disabilities (CRPD) and its Optional Protocol (OP) training aims to increase awareness of how to address discrimination using more familiar Canadian human rights laws such as Human Rights Codes and the newer international Convention on the Rights of Persons with Disabilities (CRPD). This is training for persons with disabilities by persons with disabilities. The training is part of a project funded by Employment and Social Development Canada and implemented by the Council of Canadians with Disabilities (CCD) in collaboration with Canadian Multicultural Disability Centre Inc. (CMDCI), Citizens With Disabilities – Ontario (CWDO), Manitoba League of Persons with Disabilities (MLPD) and National Educational Association of Disabled Students (NEADS). Read more.
Sign Up for our monthly digest
A monthly newsletter from CCD about what is happening in the community
CCD Submission to Special Joint Committee on Physician Assisted Dying
Related Documents
February 26, 2024
C-62: CCD, ARCH, Inclusion Canada, DAWN Canada Urged Changes to MAiD Bill - February 23, 2024
November 25, 2021
An Open Letter from the Council of Canadians with Disabilities (CCD) Concerning the Canadian Psychiatric Association Position Statement on Medical Aid in Dying (MAiD)
March 15, 2021
CCD Disappointed by House of Commons Yes Vote on Bill C-7 (Medical Aid in Dying)
January 28, 2016
Protection a Priority of the Supreme Court of Canada
The Supreme Court of Canada in Carter emphasized that there needs to be a balanced system that both enables access by patients to physician-assisted suicide and voluntary euthanasia (PAD/VE), and protects persons who are vulnerable and may be induced to commit suicide. The SCC determined that a safeguards system that imposed “stringent limits that are scrupulously monitored and enforced” would achieve this balance.1
The Council of Canadians with Disabilities (CCD) strongly believes that a minimal but mandatory vulnerability assessments, an independent review process with prior authorization, along with Criminal Code protection of the vulnerable are essential for this purpose. Without legislated requirements in the Criminal Code and clear due process, we fear there will be no reliable national standard for drawing a line around those considered vulnerable to inducement to seek PAD/VE.
Finally, CCD wants to emphasize that disability, in and of itself, is not a grievous and irremediable condition.
Vulnerability
In a request for PAD/VE, suicidal ideation, thoughts and intentions underlie that request. Even when a request is considered to be a rational, autonomously chosen act by the individual and a reasoned response to the condition of having a grievous and irremediable medical condition that causes enduring suffering intolerable to that individual, suicidal ideation underlies the request.
A question often asked is whether refusing life sustaining treatment is the same as requesting PAD/VE? The Supreme Court of Canada reasoned in Carter that:
Concerns about decisional capacity and vulnerability arise in all end-of-life medical decision-making. Logically speaking, there is no reason to think that the injured, ill and disabled who have the option to refuse or to request withdrawal of lifesaving or life-sustaining treatment, or who seek palliative sedation, are less vulnerable or less susceptible to biased decision-making than those who might seek more active assistance in dying.2
Yet the CCD understands Carter to mean that PAD/VE is to be provided only within the carved out criteria of a Criminal Code prohibition on assisted suicide. The Code is intended to protect “vulnerable persons from being induced to commit suicide at a time of weakness.” As The Canadian Association of Community Living (CACL) has stated, a person requesting PAD/VE may not be able to access PAD/VE because of the extent of their vulnerability, even if they may be able to exercise their right to refuse treatment.
CCD agrees with CACL that this legal distinction between a request for PAD/VE and the refusal of life-sustaining treatment justifies designing more robust safeguards than those now in place for withdrawing or refusing life-sustaining treatment. The Court provides the general criteria for PAD/VE in its declaration of invalidating the total ban found in the Criminal Code, by stating it was incumbent upon Parliament to design the safeguards and that “Complex regulatory regimes are better created by Parliament than by the courts.”3
Vulnerability and suffering often go hand in hand. CACL has reviewed clinical research on suicide prevention and vulnerability within the health care context, and found a wide range of factors associated with suffering that can lead to suicidal ideation and the request for PAD. Looking at the American Psychiatric Association, for example, factors that increase the risk of suicidal ideation and intent include:
- race, ethnicity and culture
- socio-economic deprivation and unemployment (for both men and women)
- sexual orientation
- major psychiatric syndrome
- specific psychiatric symptoms (anxiety, hopelessness)
- anxiety, eating and alcohol and substance abuse disorders
- physical and/or sexual abuse
- domestic violence
- family history of suicide4
Other research indicates suicidal ideation and intent is associated with:
- onset of physical disability,
For example, three major disability conditions, intellectual disability, spinal cord injury and multiple sclerosis, may make it more likely for people to consent to PAD/VE.5
The co-presence of factors in any particular case – for example, physical disability, plus isolation, plus domestic violence – increase the risk of inducing suicidal ideation and intent. Patients who come into palliative care with a long history of disability, have factors associated with their experience of prejudice, bias, disenfranchisement, and devaluation that have been shown to increase their suffering and vulnerability.6
CACL has also examined concerns about direct coercion motivating requests for PAD. Such concerns have been well documented, for example by the British Geriatric Society.7
We know that the evidence by one of the expert witnesses at the BC Supreme Court trial level of the Carter case who provided testimony regarding the legitimacy of the distinction between suffering caused by the condition/illness (such as MS) and other factors that motivate the request to die:
Professor James Werth, a Professor and licensed psychologist specializing in end-of-life counselling, deposes that, although decisions to seek hastened death may be made in difficult, emotionally-laden circumstances, nevertheless the decision-making process can be sound, rational and well-reasoned. He says that the distinction is now well established in the mainstream of psychotherapy and that “the reasoning on which a terminally ill person (whose judgments are not impaired by mental disorders) bases a decision to end his or her life is fundamentally different from the reasoning a clinically depressed person uses to justify suicide.8
The trial judge stated that “influence can be subtle and exercised at an unconscious level” and that “coercion and undue influence can be detected as part of a capacity assessment.” The Judge also noted that: “To be accurate and reliable, clinicians who perform such assessments would have to be aware of the risks of coercion and undue influence, of the possibility of subtle influence, and of the risks of unconscious biases regarding the quality of the lives of persons with disabilities or persons of advanced age.”9
Hendin and Foley, with respect to the Oregon Death With Dignity Act, conclude:
Since the passage of Oregon’s Death with Dignity Act, however, various sources patients, families, healthcare professionals, physicians, nurses, social workers, chaplains, and advocacy groups—have supplied more detailed information that suggests that the implementation of the law has had unintended, harmful consequences for patients. The Oregon law seems to require reasonable safeguards regarding the care of patients near the end of life, which include presenting patients with the option for palliative care; ensuring that patients are competent to make end-of-life decisions for themselves; limiting the procedure to patients who are terminally ill; ensuring the voluntariness of the request; obtaining a second opinion on the case; requiring the request to be persistent, i.e., made a second time after a two week interval; encouraging the involvement of the next of kin; and requiring physicians to inform [the Oregon Public Health Division] OPHD of all cases in which they have written a prescription for the purpose of assisted suicide.
The evidence strongly suggests that these safeguards are circumvented in ways that are harmful to patients. Addressing and correcting the situation would require more information than OPHD has been willing to obtain. Instead, based on the inadequate information it collects, OPHD has been issuing annual reports declaring that terminally ill Oregon patients are receiving adequate care. The available evidence, which we will present in this Article, suggests otherwise.10
Hendin and Foley also examined the data gathered by the Oregon Public Health Division (OPHD) and stated the following:
The OPHD annual reports are marked by overreaching in the conclusions they draw from the limited information they have. As we have previously discussed, most striking and least justified has been OPHD’s contention, without substantiating data, that patients who have requested assisted suicide were receiving adequate end-of-life care. Data from Oregon investigators, surveys of and interviews with families who observed the pain or distress of their relatives who received end-of-life care, new surveys of nurses who cared for hospice patients, and new surveys of physicians’ experiences do not support this contention.11
Hendin and Foley looked at the issue of alternatives to PAD, and how psychiatric illness, voluntariness and coercion act as limits to physician liability. They also examined the role of non-government agencies like Compassionate in Dying. Serious concerns were raised in this article with respect to the issue of autonomy and control:
... what is most likely to increase the demand for assisted suicide is the impetus to treat the question as one of autonomy and control. Oregon has been in the forefront of this trend. The original impetus for passage of the Oregon law was to help relieve intractable symptoms such as pain, but as the law was written and monitored it has evolved into providing an option for control. Oregon physicians report that the most common reason patients request PAS is not pain or depression but a need for control. This need is usually related to patients’ fears of the future and presents the physician with an opportunity to address their specific concerns and to develop interventions that will relieve the anxiety of most patients. Oregon researchers have described these patients, noting that they were inflexible and “dreaded the thought of being dependent on others.”
The need for control, however, is characteristic of most suicidal patients. They make absolute conditions on life: “I won’t live . . . without my husband,” “if I lose my looks, power, prestige, or health” or “if I am going to die soon.” Depression, often precipitated by discovering a serious illness, exaggerates their tendency to see life in black and white terms, but for most such people the need for control has been a dominant feature of their lives. They are unable to tolerate dependency on other people. In any case, the good practice of medicine obliges doctors to relieve distress rather than to assume that hastening death is the best or only way of doing so.12
RIGHT TO PALIATIVE CARE
The report from the Royal Society of Canada Expert Panel: End-of-life Decision Making13 , suggests that permitting PAD/VE would not necessarily lead to a reduction in resources for palliative care and for adapting various social context and institutions although it does state that this fear is not unfounded.14 Its suggested remedy is to have legislation requiring the funding of such programs as palliative care.
CCD puts forth the need to establish the means to provide Canadians with adequate palliative care, which to this day is not covered under the Canada Health Act, and is acknowledged to be available to only a minority of Canadians who require it.
The Honourable Sharon Carstairs’ 2010 Senate Report, Raising the bar: A Roadmap for the Future of Palliative Care in Canada, recommends, among other things, the following:
- The establishment of a Canadian Strategy on Palliative Care as a partnership between the federal, provincial and territorial governments and the community which would pave the way for consistent minimum standards and benchmarks for nationally available palliative care services;15
- Establish a Canadian Palliative Care Capacity Building Fund;16
-
The provinces ensure that Palliative Care are covered under all provincial and territorial health insurance plans;17
CCD asserts that the crossover between the request for PAD/VE and the lack of access to palliative care is clear.
Vulnerability Assessments
The above articulates the reasons CCD is requesting vulnerability assessments that will determine if a person meets the criteria set out in the Carter case. Carter acknowledged that any set of safeguards must recognize the complex and sometimes very subtle and subconscious factors related to a request for PAD/VE. This confirms the requirement for a vulnerability and capacity assessment process.
People are made vulnerable as a result of social or economic circumstances that diminish their resiliency. Conditions such as poverty, isolation, discrimination, devaluation and lack of needed supports are therefore highly relevant in determining whether a person may be vulnerable to inducement.
CACL has looked at sources of vulnerability which include:
- Inherent vulnerability (e.g., to a grievous and irremediable condition/illness)
- Situational vulnerability (e.g., to a particular confluence of factors related to suicidal ideation and intention)
- Pathogenic vulnerability (e.g. to dysfunctional, abusive, exploitative relationships)18
Vulnerability assessments could be positioned in the informed consent process as follows (From CACL):
a. Patient makes request to responsible physician
b. Medical condition/suffering is assessed to see if it meets criteria as per Carter and if the individual is vulnerable.
c. If yes to possible vulnerability, the responsible physician engages a qualified professional such as a psychologist, social worker or other qualified regulated professional designated for this purpose. The assessment of vulnerability factors includes, suicidal ideation and intent, patient-reported health care outcomes, and assessment of patient resiliency. It helps to ensure that the consent is free, non-ambivalent and voluntary, and protects against any conflicts of interest in the health care system.
d. This qualified professional is a separate health professional, thus helping protect against any criminal liability for proceeding with PAD/VE when a person may have been vulnerable to being induced. If ‘no risk’ determined, then the physician completes the informed consent inquiry and proceed to advance independent authorization.
If vulnerability is found then the evidential standard for the vulnerability to not have an impact on the request for PAD/VE must be a “clear and convincing” standard. Without such attention to the impact of vulnerability, there is very real risk that people will die in a manner that violates criminal prohibition.
The Review Board Process
The vulnerability assessment, along with the assessments of two physicians, is submitted with the application by the patient requesting PAD/VE to a Review Board. It is a Review Board or a nationally constituted Board, and not a physician, that would make the ultimate determination on whether a request for PAD/VE will be granted.
CCD agrees with Baker, Sharpe and Lauks19 , that each panel of the Review Board should be chaired by a federally appointed Judge to ensure consistency in reasons for judgments and the review process should be in place in order to facilitate Canada-wide standards based on the undefined and general criteria supplied by the Supreme Court of Canada and not have access based on provincial standards set by each province or by individual physicians.
If the criteria are not met and the physician goes ahead with the request, the physician can be charged and convicted under the Criminal Code. Parliament must, through its legislative revision of the Criminal Code specify the safeguards and criminal sanctions against assisted suicide in order to distinguishing between a legal request for PAD/VE and a criminal act.
Appendix A
Fundamental Principles
- A national, comprehensive, regulatory system is required to protect persons who are vulnerable to being induced to commit suicide in times of weakness.
- People with disabilities are at greater risk of vulnerability because of the emphasis on compliance with caregivers and similar authority figures. This is especially true of people with intellectual disabilities, people with a lived experience of mental illness and survivors of trauma.
Guidelines for Legislative and Policy Response
1. A definition of the terms PAD/VE, should be included in the legislation, especially with respect to the exclusion of disability.
2. PAD/VE must be available only to competent adults with a grievous and irremediable condition that is the cause of enduring suffering that is intolerable to the individual.
3. There must be national funding and provincial involvement in a palliative care application, that is, palliative care must be considered an insured benefit.
4. Requests for physician-assisted suicide must be reviewed and authorized by an independent review panel with sufficient information to determine if the necessary criteria are met.
5. In making its decision the review panel must consider the following information:
a. The person’s request and reasons for the request;
b. A clinical evaluation by two qualified physicians regarding whether the person meets the medical criteria;
c. A clinical evaluation by two qualified physicians regarding whether the person’s condition is irremediable in the sense that it is likely to cause death within the foreseeable future. Where this prognosis is not the case, special inquiry must be made into whether there are conditions that place the person at risk of being vulnerable to being induced to commit suicide, and whether all alternative courses of action have been considered;
d. A clinical evaluation by two qualified physicians that the person is competent to make the decision;
e. An assessment and documentation by two physicians stating whether or not the person’s request is informed and voluntary;
f. The patient must be informed of potential alternative courses of action that might reduce the person’s suffering. This information must be conducted by a qualified professional (physician) in consultation with the patient, and must address a full range of alternatives to PAD/VE including medical treatment, palliative care, counselling and disability related supports. PAD/VE can only be made available after a detailed and individualized plan for high quality palliative care has been thoroughly presented, considered and refused;
g. Accommodations must be made for linguistic barriers for Deaf and hard of hearing people, Deaf/Blind people, Blind people, people with low vision and people with speech difficulties;
h. A full explanation of the risks and complications of PAD/VE must be provided as a part of informed consent.
i. Submissions by third parties with direct knowledge relevant to the request, subject to the discretion of the review panel.
j. Clinical input to the review panel process must come from at least two different physicians.
6. A monitoring system and annual public reports to Parliament and provincial/territorial legislatures must be in place to track and report on:
a. the number of requests;
b. the reasons given;
c. using aggregate data gender, medical condition, socio-economic circumstances and demographic factors associated with persons making requests, and those whose requests are authorized or denied;
d. availability and acceptance or refusal of alternative courses of action identified;
e. efficacy of alternative interventions including access to medical treatment and palliative care;
f. outcome of requests authorized and denied;
g. create a mechanism for families and other interested parties to call for an investigation.
7. Measures to be taken in the event of improper use of physician assisted death include.
a. Compensation to the estate and/or family members of those who were found to be wrongly given physician assisted death;
A mechanism of intervention from interested parties who are concerned about the possibility of coercion or discrimination; and enforcement under the Criminal Code.
Endnotes
1. Carter v. Canada (Attorney General), 2015 SCC 5 at para 105, citing the earlier BC Supreme Court Decision.
2. Carter v. Canada (Attorney General), 2015 SCC 5 at para 115.
3. Carter v. Canada (Attorney General), 2015 SCC 5 at para 125.
4 . D Russell, RJ Turner and TE Joiner. (2009). Physical disability and suicidal ideation: a community-based study of risk/protective factors for suicidal thoughts, Suicide and Life-threatening Behaviour V. 39 (4), 440-451.
5. MJ Gianni, B Bermark, S Kreshover, E Elias, C Plummer and E O’Keefe. (2010). Understanding suicide and disability through three major disabling conditions: intellectual disability, spinal cord injury and multiple sclerosis, Journal of Disability and Health 3(2),. 74-78.
6. D Stienstra and HM Chochinov. (2006). Vulnerability, Disability, and Palliative End-of-Life Care, Journal of Palliative Care (22, 3, Autumn).
7. British Geriatrics Society.(2004). Assisted dying for the terminally ill Bill BGS response to the House of Lords.
(Online: http://www.bgs.org.uk/Publications/Position%20Papers/psn_terminally_ill_...).
8. Carter v. Canada (Attorney General), 2012 BCSC 886, at para 813.
9. Carter v. Canada (Attorney General), 2012 BCSC 886, at para 814.
10. K Hendin and H Foley. (2008). Physician Assisted Suicide in Oregon, Michigan Law Review 1613 - 1639, 1614.
11. Ibid, 1636-1637.
12. Ibid, pages 1635 and 1636.
13. Schüklenk, U., Van Delden, J. J., Downie, J., Mclean, S. A., Upshur, R., & Weinstock, D. (2011). End‐of‐Life Decision‐Making in Canada: The Report by the Royal Society of Canada Expert Panel on End‐of‐Life Decision‐Making.
14. Ibid at page 67
15. S. Carstairs, (2010). Raising the bar: A roadmap for the future of palliative care in Canada. Senate of Canada. page 47, recommendation 1.
16. S. Carstairs, (2010). Raising the bar: A roadmap for the future of palliative care in Canada. Senate of Canada.page 48, recommendation 8.
17 S. Carstairs, (2010). Raising the bar: A roadmap for the future of palliative care in Canada. Senate of Canada. page 48, recommendation 13.
18. States of vulnerability
• Dispositional (that the range of inherent, situational and pathogenic factors have some degree of potential to make one vulnerable to the risk of being induced to commit suicide in a time of weakness)
• Occurrent (that the range of situational and pathogenic factors are making one vulnerable to the risk of being induced to commit suicide in times of weakness).
19 D Baker, G Sharpe and R Lauks. (2015). “FEDERAL AND PROVINCIAL RESPONSIBILITIES TO IMPLEMENT PHYSICIAN ASSISTED SUICIDE”.
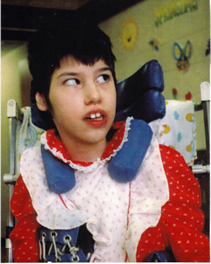
Tracy Latimer
The Latimer Case
The Latimer case directly concerned the rights of persons with disabilities. Mr. Latimer's view was that a parent has the right to kill a child with a disability if that parent decides the child's quality of life no longer warrants its continuation. CCD explained to the court and to the public how that view threatens the lives of people with disabilities and is deeply offensive to fundamental constitutional values. Learn more.
